Stress is more often than not a term that we associate with the negative aspects of our lives; money worries, work life, job security, the list goes on and on. Indeed, there are a huge number of things that can contribute to negative stress. But is there more to stress than meets the eye?
This blog is provided by Dr John Briffa; a practising doctor, author and international speaker. Dr Briffa explores the good and the bad sides of stress, introducing some of the strategies that can be used yourself, or with clients, to boost resilience and help to maintain balance and wellbeing.
The science of stress and resilience
For many, the word ‘stress’ has negative connotations. Not uncommonly, it is viewed as unwanted and unhealthy psychological and physiological effects generated by the ‘stresses’ and challenges we encounter in our lives.
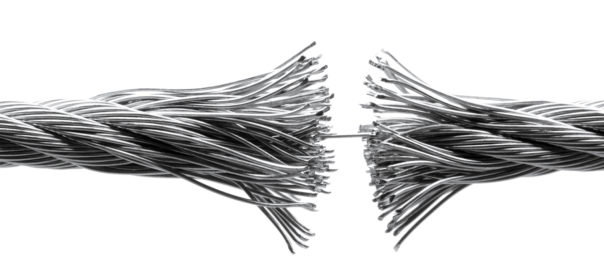
But while it’s true that excessive stress can have negative consequences for our emotional and physical wellbeing, some stress can undoubtedly be a good thing. At a most fundamental level, stress energises both the body and brain, prepares us for action and can boost performance. Plus, as Miguel Toribio-Mateas pointed out in his recent Cytoplan blog, stress can lead to ‘growth, adaptation and new learning’. Stress is very much a double-edged sword.
This blog post will explore some of the good and bad of stress. It will also introduce some ideas and strategies that we can use personally (or with clients) to boost resilience and help maintain balance and wellbeing, even ‘when the pressure is on’.
The Stress Response
Our response to stress, whether it be psychological or physiological in nature, is mediated via neurological and hormonal (endocrinological) systems.
The Neurological Stress Response – the Sympathetic Nervous System
The nervous system in the body is broadly divided into two parts; the voluntary (or ‘somatic’) nervous system that controls conscious actions such as walking and talking, and the autonomic nervous system that controls functions not generally under our conscious control such as our heart rate, breathing rate, blood pressure and body temperature.
The autonomic nervous system is sub-divided into two parts, known as the sympathetic and parasympathetic nervous systems. The sympathetic nervous system is usually activated in response to any stress (be it psychological or physical) and, among other things, speeds up the heart and breathing rate.
The parasympathetic nervous system has the opposite effect, and tends to be activated when we are resting or recovering (as well as during digestion). A simple analogy is to think of the sympathetic and parasympathetic nervous systems as the body’s ‘accelerator’ and ‘brake’ respectively.
The Hormonal Stress Response – the Adrenal Glands
The hormonal response to stress in the body is mediated through what are known as the adrenal glands, which sit on top of the kidneys. Stress sensed in the brain leads to the release of hormones that ultimately cause the adrenals to secrete two main ‘stress hormones’: adrenaline and cortisol.
Adrenaline is a relatively short-acting hormone that, among other things, speeds the heart, raises blood pressure, and increases blood levels of glucose and fatty acids (providing ready fuel for energy).
Cortisol is a longer-acting hormone, and has similar actions to adrenaline, but in excess in the long term can predispose to fat deposition (particularly ‘abdominal’ weight gain), muscle loss, immune suppression and damage to the brain (particularly a brain structure known as the hippocampus, which plays a role in functions such as memory consolidation and spacial memory).
There’s no doubt that there are two sides to the stress coin. In the short term stress energises the body and essentially puts us in a state where we can more effectively ‘rise to the challenge’. However, it’s equally true that overwhelming or unremitting stress can have quite devastating effects on our physical and psychological wellbeing.
One of the risks of long-term stress is a weakening of adrenal gland function, for which the term ‘adrenal fatigue’ has been coined. Characterised by dysfunction in the secretion of cortisol and/or another major adrenal hormone (DHEA), this syndrome can give rise to symptoms and signs such as low energy, easy fatigue, mood issues and sleep problems. My own experience tells me that adrenal fatigue is a common underlying factor in individuals suffering from issues such as unexplained fatigue and chronic fatigue syndrome (CFS).
In short, in relation to stress, ‘we can get too much of a good thing’. What approaches can we take, then, to ensure we make the best of stress and protect ourselves from potential issues in the short- and long-term?
Maintaining Balance in the Autonomic Nervous System
While activation of the sympathetic nervous system certainly has its place in appropriate circumstances, as a general rule it makes sense to ensure this activation does not go on for too long or happen too often. Some of the approaches that have considerable potential to ‘keep a lid’ on stress essentially activate the parasympathetic nervous system, thereby dampening sympathetic nervous system activity.
One function that has significant relevance here is breathing. There is a tendency for some of us, particularly in times of stress, to breathe relatively quickly and mainly from the chest (sometimes referred to as ‘hyperventilation’ or simply ‘over-breathing’). Some of the effects of hyperventilation include:
- Lower-than-ideal levels of carbon dioxide levels in the bloodstream, which in turn can compromise oxygenation of tissues and organs (including the brain), due to something known as the Bohr effect.
- Blood vessel constriction, compromising circulation including to the brain (and essentially starving the brain of oxygen and key nutrients).
- Lower blood calcium levels, causing symptoms such as numbness and muscle spasms (particularly in the hands and feet).
- Elevated levels of lactic acid in the blood, which itself can provoke symptoms of anxiety and panic (particularly in individuals prone to these symptoms).
While relatively few people suffer from breathing so dysfunctional that they suffer from full-blown panic attacks, my experience in practice is that many more experience undue anxiety, restlessness and ‘stress’ primarily as a result of a tendency to dysfunctional breathing.
Many individuals in this situation seem to benefit very quickly from practising specific breathing exercises even on a semi-regular basis. Breathing more from the diaphragm or ‘belly’ (rather than the chest) is key here, as is taking slower breaths (around six breaths per minute appears to be generally effective). Just these things alone help to stimulate the parasympathetic nervous system1, and also correct the biochemical and physiological imbalances and ‘stresses’ typical in dysfunctional breathing.
But there are many other approaches that can be taken on a daily basis that strengthen the parasympathetic nervous system and, in so doing, help to provide an effective buffer against stress. For example, intermittent fasting, cold exposure and singing all have the capacity to influence parasympathetic activity..
Keeping track of stress
We can get a pretty good idea of the relative activity in the sympathetic and parasympathetic nervous system from a measure known as ‘heart rate variability’ (HRV). This metric essentially tells how much variation there is in the pause between individual heart beats. Low- and high-HRV generally signal sympathetic and parasympathetic dominance respectively.
There are now available quite simple and affordable technologies that we can use to track HRV, effectively providing a window into the activity and balance in our autonomic nervous system at any point in time. This technology can also be used to help us train our ability to control stress better and monitor the effects of any changes we make.
Looking after the adrenals
Any approach that reduces activation of the ‘stress response’ helps, in its own way, to support and preserve the function of the adrenal glands. However, a more direct approach can be taken here too in that certainly lifestyle nutritional and lifestyle factors (including good quality sleep) can support adrenal health and recovery. In addition, support for the adrenals can come in the form of specific nutrients and herbs including vitamin B5, ginseng, liquorice, ashwagandha and rhodiola.
Mind Control
A combination of these approaches, tailored to the needs of individuals, can improve wellbeing and resilience. But none of them immunise us from the fact that life can be unpredictable and ‘bad things can happen’. Being resilient physiologically can certainly help ensure we respond appropriately to life’s challenges, but shifts in mindset and thinking at ‘difficult times’ may also do much to ‘take the stress off the system’. What mental approaches may ‘diffuse’ negative emotions such as sadness, anxiety and fear?
Potential here comes from the fact that emotions do not come from nowhere: They are generated in response to the beliefs we have about our experiences or situation. If our belief is that something is ‘bad’, then ‘stress’ and ‘negative emotions’ are the likely result. If we were to change our beliefs to something more positive, then the outcome may be much more positive too.
Some may argue that our beliefs are based on ‘the facts’. But another point of view is that nothing has any inherent meaning, only the meaning we ascribe to it. As Shakespeare’s penned (in Hamlet), ‘… there is nothing either good or bad, but thinking makes it so.’
Whatever meaning we give to an event or situation is likely influenced by things like our habitual thinking and ‘conditioning’ from influences such as parenting, education, and ‘societal norms’. The way these differences mould our thinking at least in part explains why two different people can see the same situation in quite different ways. And the fact that someone can find themselves having very different responses at different times to essentially the same situation demonstrates that these beliefs are potentially malleable.
In times of the challenge, what’s ‘stressing us out’ is not necessarily the event or situation we face per se, but how we are viewing and approaching it. This concept is not new: almost 2,000 years ago the Greek philosopher Epictetus had it that ‘Men are disturbed not by things, but by their opinions about them.’
Looking at a situation in a different way and reaching for beliefs and ideas that work better for us can do much to ‘take the sting out of’ a supposedly challenging situation. It may also facilitate our learning and growth, and help us derive benefit from the experience.
Mindset Matters
An example of the importance of how our thinking and mindset affects health concerns stress itself. In one study, individuals who had experienced a lot of stress over the preceding year were found to be at significantly enhanced risk of death over time. However, this increased risk was limited to individuals who had clear belief that stress has negative effects on health. Interestingly, in those who had also endured a lot of stress over the past year but who had little or no concept that stress affects health saw no increased risk of death.2
This study is ‘epidemiological’ in nature, and therefore cannot tell us whether the generally negative attitude to stress actually caused the enhanced risk of death. However, evidence for a direct relationship between stress mindset and health has come from other work. In one study, individuals were exposed to 3 brief videos espousing the ‘stress-is-enhancing’ concept over the course of a week. Compared to those exposed to ‘stress-is-debilitating’ videos or no videos at all, these individuals subsequently went on to enjoy improved health status and enhanced work performance.3
Our response to stress and our resilience partly depends on physiological factors that are largely under our control. And the same is true for the mental and psychological approaches we can take to the challenges we face in our lives.
Dr John Briffa BSc (Hons) MB BS (Lond)
 Dr John Briffa is a practising doctor, author and international speaker. He is a prize-winning graduate of University College London School of Medicine, where he also gained a BSc degree in Biomedical Sciences. Dr Briffa is a leading authority on the impact of nutrition and other lifestyle factors on health and illness. He is dedicated to providing individuals with information and advice they can use to take control of their health and optimise their energy and vitality.
Dr John Briffa is a practising doctor, author and international speaker. He is a prize-winning graduate of University College London School of Medicine, where he also gained a BSc degree in Biomedical Sciences. Dr Briffa is a leading authority on the impact of nutrition and other lifestyle factors on health and illness. He is dedicated to providing individuals with information and advice they can use to take control of their health and optimise their energy and vitality.
Dr Briffa is a former columnist for the Daily Mail and the Observer, and former contributing editor for Men’s Health magazine. He has contributed to over 50 newspaper and magazine titles internationally, and is a previous recipient of the Health Journalist of the Year award in the UK.
With many thanks to Dr John Briffa for this article. If you have any questions regarding the topics that have been raised, or any other health matters please do contact me (Clare) by email at any time.
clare@cytoplan.co.uk
Clare Daley and the Cytoplan Editorial Team
References
- Pal GK,, et al. Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res.2004;120(2):115-21
- Keller A, et al. Does the perception that stress affects health matter? Health Psychology 2012;31(5):677-84
- Crum AJ, et al. Rethinking stress: The role of mindsets in determining the stress response. Journal of Personality and Social Psychology 2013;104(4):716-733
Last updated on 25th March 2019 by cytoffice


Stress and adversity are a part of work life but being able to manage a stress generating event to allow for some prospect and flexibility will help to build a health resilience.
Regards,
John Lyman
It is very hard for me to see any positive side to the stress associated with caring for a demanding, often aggressive, disabled husband with Apergers and signs if dementia. Perhaps Dr Briffa can suggest ?
Dear Veronica-Mae
Thank you for your comment on our blog. There are of course many life circumstances where it can be difficult to manage associated stress, I am sorry to hear of your difficulties. As you probably know, caring roles are associated with high levels of stress and increased inflammation in the body and carers may overlook their own needs. I hope you are able to support yourself as much as possible – you might benefit from some professional help e.g. CBT which might be available to you via your GP. Alternatively my suggestion would be NLP / Hypnotherapy with a professionally qualified therapist.
Social support is also important. There is a good website – where you can find local groups that share your interests, meetups are usually free and provide a huge range of social opportunities. Local dementia support groups are also be worth considering.
In addition to this there are a couple of techniques that you can do at home.
– Gratitude Journal: A very simple measure you can use at home which has been shown to increase happiness within 7 days, is keeping a Gratitude Journal – this is where make a written note of at least 3 positives from the day. The key here is to find at least 3 positives from every day, even on really bad days, they can be little things e.g. it was a sunny day or I enjoyed a lovely cup of coffee in a café or I had a friendly conversation with checkout lady etc. I recommend this is done at bedtime so that you reflect before sleep on some positives from your day.
– 4/7 breathing – this is a type of breathing that has been shown to switch on the relaxation response. Breathe in slowly through your nose to the count of 4, pause, then breathe out slowly through your mouth to the count of 7. Repeat this 12 times. Aim to do this every day at least once, regardless of whether you are feeling stress. I hope you don’t think this suggestion is glib – – I have recommended. This has been shown to increase happiness levels within 7 days. a stranger smiled at me.
Exercise, diet and adequate sleep are also really important to help you cope with stress. With regard to diet if you can aim for a low sugar diet, with lots of vegetables (aim for variety) and healthy fats (olive oil, nuts, seeds, avocado, oily fish), include some good quality protein at each meal. If you would like some more tailored diet and supplement recommendations please complete a health questionnaire and we will send you some written recommendations. This is a free service.
Wishing you all the best
Clare