In this week’s blog, our Nutritional Therapist, Ruth, explores in detail all things gamma linolenic acid. GLA for short!
What is GLA?
Gamma-linolenic acid (GLA) is an omega-6 fatty polyunsaturated fatty acid (PUFA). Omega-6 fatty acids are considered essential fatty acids, as they are necessary for human health, but the body cannot make them. You therefore need to get them through diet. Along with omega-3, omega-6 PUFAs play a crucial role in brain function, and normal growth and development. Both omega-3 and omega-6 PUFAs regulate inflammation, immunity, blood vessels, platelets, synaptic plasticity, cellular growth, pain, sleep and many other bodily processes8.
Over the last few decades, the publicity in the area of healthful fatty acids has been dominated by omega-3 fats, and more specifically EPA and DHA found in oily fish. This publicity is based on a large body of scientific evidence that links omega-3 fatty acids to a decreased risk of several chronic diseases such as cardiovascular disease, diabetes, cancer, cognitive decline, depression, as well as a supportive role in visual and neurological development, and maternal and child health1.
Omega-6 fatty acids: Health threat or health friend?
Evidence on the health benefits of omega-3 PUFAs very often depicts omega-6 fatty acids in a negative light; even as a potential health threat. The basis for this conclusion is the evidence that an imbalanced ratio between omega-6 to omega-3 fatty acids can lead to a range of health concerns4-6. The average ratio of omega-6: omega-3 in the Western diet is approximately 20:1, whereas in the palaeolithic times (and up to around 100 years ago) the ratio was thought to be closer to 4:16.
Omega-3 and Omega-6 fatty acids ratio in modern day dietary intake
One reason for this imbalanced ratio is the low intake of oily fish in the Western diet, coupled with a high dietary intake of the omega-6 fatty acids linolenic acid (LA) and arachidonic acid (AA).
Because it is synthesised in plants, LA is found in high proportions in foods of plant origin. For example, many seeds, nuts, and plant oils are rich in LA; these include safflower, sunflower and pumpkin seeds, walnuts, corn, and sunflower, safflower and soybean oils2.
Conventionally reared meat, such as chicken and pork are often fed a diet high in LA, including corn and soy, and thus contain high levels of omega-6 fatty acids in their meat7.
For the last few decades, following widespread recommendations to eat unsaturated fatty acids as opposed to saturated fatty acids, intake of fatty acids in modern society has been shifted from saturated fatty acids (butter, lard) to vegetable oils rich in LA and poor in omega-3 fatty acids8, which is likely to be one of the reasons that led to a remarkably significant increase in the ratio of omega-6/omega-3.
LA and AA combined account for the majority of omega-6 dietary intake, to which the potential negative effects of the imbalanced fatty acids ratio are linked.
GLA, however is only present in small amounts in the diet but has the potential to have similar benefits to omega-3 fatty acids – evidence of which we will discuss below.
GLA is present in some plant seed oils including evening primrose, blackcurrant, and borage oils (where it contributes about 9%, 17%, and 21% of fatty acids, respectively)3.
Fatty acids, inflammation and prostaglandin creation:
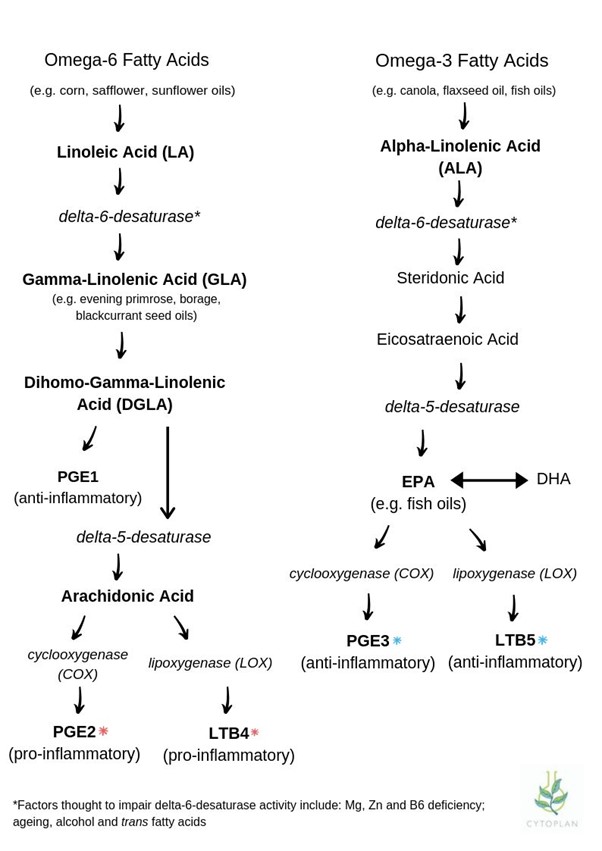
One of the key compounds generated from fatty acids are hormone-like substances called prostaglandins. The primary role of prostaglandins is to support the healing process by balancing inflammatory and anti-inflammatory processes. They are found in almost every cell and tissue throughout the body and are essential to proper functioning.
The three major prostaglandins in the body include PgE1, PgE2 and PgE3:
- PgE1 (anti-inflammatory) – formed from omega-6 fats; either LA or GLA sources
- PgE2 (inflammatory) – primarily derived from AA
- PgE3 (anti-inflammatory) – formed from omega-3 fats; either ALA or more directly from EPA sources
GLA is converted into ‘dihomo’ GLA or DGLA and this is incorporated into cell membrane phospholipids. GLA is metabolized into prostaglandin E1 (PGE1), a potent anti-inflammatory mediator that can modulate immune responses and reduce inflammation9.
PgE1 is the most potent anti-inflammatory prostaglandin in the body. It is produced through the metabolism of LA into GLA, however this reaction is slow and can be impaired by a variety of factors such as stress, poor diet and various medications. Furthermore, proper digestive, liver and enzymatic function are essential for ensuring that the fats consumed in the diet can be converted into prostaglandins. By directly supplementing with GLA, one can bypass this inefficient conversion process, ensuring a more reliable and effective increase in DGLA levels.
GLA can support a balanced level of inflammation in the body through a process called competitive inhibition; DGLA competes with AA for access to enzymes (i.e., cyclooxygenase and lipoxygenase) that create prostaglandins that either promote or resolve inflammation11.
This means that the presence of DGLA in tissues can help lower the output of AA’s prostaglandins by inhibiting their production and/or blocking their transformation13, which ultimately translates to lower levels of pro-inflammatory prostaglandins.
It is important to note that both inflammatory and anti-inflammatory prostaglandins are essential, it is only when the system falls out of balance and creates too much PgE2 at the expense of PgE1 and PgE3 that issues arise. Omega-3 and omega-6 PUFAs compete for the same conversion enzymes and so consuming a high level of dietary omega-6 may cause issues even in the context of high dietary omega-3.
What is GLA good for?:
As we have explored, GLA is a unique omega-6 PUFA, which demonstrates a variety of anti-inflammatory properties. The idea that we don’t require GLA due to the high amounts of omega-6 consumed in our diet is a common misconception, when in fact, GLA is vital in order to neutralise and reverse the effects of an excess of AA and LA fatty acids in the diet.
GLA has been used for centuries as part of homeopathic remedies, however, it is only in recent years that the research has caught up and several benefits have been confirmed and discovered:
GLA & hypertension
In one study on post-menopausal women with hypertension, those who received supplementation of 1000mg borage oil, rich in GLA over a 6-month period, saw a significant reduction in the systolic and diastolic pressure as well as a significant change in waist-hip ratio10.
Gamma linolenic acid & diabetes mellitus
The prevalence of type II diabetes is increasing worldwide and has the potential to affect different organs such as the kidney, brain, heart, amongst others, in chronic stages. A decrease in insulin activity has the potential to reduce delta-6 desaturase and impair the conversion of LA to GLA16. This phenomenon has a key role in membrane structure and 6-desaturated metabolites, the precursors to prostaglandins.
All of these can lead to cardiovascular complications alongside diabetes, and consequently it has been suggested that high doses of GLA be effective in neuropathy improvement and cardiovascular disorder risk reduction in the condition16.
Neuropathy is the most common complication among diabetes patients15. GLA is an essential component of structural phospholipids in neural cell membranes and, as such, is necessary for the maintenance of normal nerve membrane structure and function. One study measured the efficacy of GLA for reducing pain severity in diabetic neuropathy over a 12-week period and concluded that it offered a well-tolerated and effective treatment option15.
GLA & rheumatoid arthritis (RA)
RA is one of the most common autoimmune conditions, characterised by pathological changes in the lining of the joints. In RA, the overproduction of the inflammatory molecules PGE2, tumour necrosis factor (TNF), interleukin (IL)-1, and cytokines induce the chronic inflammation that causes pain and swelling in the joints. Several clinical trials have demonstrated a beneficial effect of GLA in alleviating inflammation and disease severity in RA17.
Gamma linolenic acid and skin health
In one interventional study, 40 men and women received either 1.5g GLA-rich evening primrose oil or placebo. After 12 weeks, those receiving evening primrose oil had significant improvements in skin moisture, elasticity, firmness and trans-epidermal water loss (a measure of barrier integrity) compared to placebo21. There is also evidence of GLA supporting specific skin conditions:
Atopic eczema
Atopic eczema is a chronic inflammatory skin condition, which usually develops in early childhood and can have a significant impact on quality of life. The pathology of atopic eczema is multifactorial and has complicated immunological abnormal responses, including damage to the epidermal barrier, genetic factors, and environmental causes.
Some researchers have suggested that atopic eczema may be related to the abnormal metabolism of essential fatty acid, especially in the production of gamma-linolenic acid, and a functional deficiency in delta-6 desaturase has been identified, leading to a decrease in GLA, and consequently a dominance of inflammatory prostaglandins18.
Supplementing with evening primrose oil, a rich source of GLA has demonstrated improvements in the severity of eczema symptoms19. Some studies suggest balancing a typical western diet, rich in LA and AA, with GLA and omega-3 fatty acids, which can act to balance the fatty acid composition of membrane phospholipids and/or inhibit the production of proinflammatory eicosanoids20.
Acne
Acne is a common, inflammatory skin condition characterised by excessive sebum production, follicular hyperkeratinisation of sebaceous ducts, and an increased release of inflammatory mediators. It has been estimated that approximately 85% of adolescents have acne; however, this dermatosis may occur in childhood and can persist beyond adolescence.
GLA is thought to be supportive in acne, not only due to its anti-inflammatory properties, but also since DGLA can reduce follicular hyperkeratinisation22.
One study found that GLA from borage oil was comparable to EPA and DHA for improving acne lesions and found that it presented a safe and tolerable adjuvant treatment for mild to moderate acne23. GLA has also shown to have a protective role on the skin barrier and maintains skin hydration in those who are treated with the acne medication isotretinoin22.
There are more and more promising studies in favour of combined GLA and omega-3 PUFAs supplementation showing the highest potential in diminishing inflammatory processes and ameliorating chronic inflammatory skin diseases22.
GLA & female health
Premenstrual Syndrome (PMS)
PMS is a condition, which is associated with somatic, emotional and behavioural symptoms before or during menstruation. Anxiety, depression, acne, fatigue, and headache are common symptoms of PMS and around 85% of women of menstrual age are thought to be affected by the condition.
Low levels of PgE1, as the result of a deficiency in essential fatty acids is thought to cause high sensitivity to prolactin, and high prolactin levels throughout the menstrual cycle, which is thought to contribute to the symptoms of PMS24.
One review of the research highlighted eight studies that compared evening primrose oil with a placebo for PMS and one study comparing GLA with a placebo. The evening primrose oil study showed a significant decrease in PMS severity, while the GLA study showed a shortened duration and decreased severity of PMS symptoms24.
Mastalgia
Mastalgia, or breast pain, is a common condition among premenopausal women, which can lead to significant impairment in daily living. The pathology of cyclical mastalgia is likely to be multifactorial and include hormonal fluctuations (particularly variations in oestrogen and progesterone), breast tissue sensitivity, inflammation, cyclic changes in breast anatomy, psychological factors, nerve sensitivity, and fibrocystic changes25.
GLA’s beneficial role in mastalgia is thought to be due to its ability to modulate prostaglandin synthesis and promote hormonal balance, thus alleviating breast pain25.
Gamma linolenic acid, menopause transition and post-menopause
Menopause is a natural transition in a woman’s life that typically takes place between the ages of 45 and 55 and is triggered as a woman’s oestrogen levels begin to decline. For many women this natural stage in life can become a time of physical and emotional discomfort, and the most common symptoms include hot flushes, night sweats, insomnia, anxiety, mood swings and weight gain.
As mentioned, GLA authorises the synthesis of anti-inflammatory substances such as 15-hydroxy-eicosatrienoic acid and prostaglandin E. Prostaglandins function as central neurotransmitters and influence the hypothalamic pituitary axis, and GLA is thought to help counter menopausal hormonal changes by increasing the production of prostaglandins27.
One study, examining the effects of evening primrose oil on hormonal levels in menopause found a decrease in follicle stimulating hormone, and increase in oestradiol and improvements on the “menopause rating scale” after 2 months of use27.
Another study demonstrated improved mood and decreased psychological symptoms such as low mood, irritability, anxiety and mental exhaustion upon taking evening primrose oil. The authors suggest that this is likely to be due to the high level of GLA in the oil26. Evening primrose oil has also shown improvements in the severity of hot flushes in post-menopausal women28.
Gamma linolenic acid and neurodivergence
There is a wealth of evidence of a supportive role of PUFAs in neurodivergent conditions such as attention deficit hyperactivity disorder (ADHD). Evidence has typically focused on omega-3 PUFAs, but a supportive role of GLA in neurodivergence is emerging.
Due to its anti-inflammatory properties, GLA has demonstrated a supportive role in ADHD and associated symptoms, particularly when it is combined with omega-3 PUFAs.
In particular, a combination of EPA and DHA with the addition of GLA in a 9:3:1 ratio appears to be associated with improvements in ADHD symptoms. It is hypothesised that this may be due to omega-3 PUFAs preventing the accumulation of serum AA in response to GLA12.
Gamma linolenic acid and children’s health
When combined with an omega-3 fish oil and vitamin D supplement, GLA from blackcurrant seed oil demonstrated benefits in children with atopic dermatitis after 4 months of treatment. The benefits included a significant reduction in eczema symptoms, a reduced need for topical corticosteroids and improvements in itch, sleep quality, and overall quality of life14. This combination has been suggested as a safe and effective intervention that may help to reduce the severity of symptoms of atopic eczema in children.
Key takeaways
- Gamma-linolenic acid (GLA) is an omega-6 fatty polyunsaturated fatty acid
- Along with omega-3 fatty acids, omega-6 is essential for human health and supports a number of different bodily processes
- Some omega-6 fatty acids, when taken in excess, can promote an inflammatory state, but GLA, in contrast, possesses anti-inflammatory properties
- This anti-inflammatory effect is more pronounced when GLA is combined with the omega-3 fatty acids EPA and DHA
- GLA has shown a supportive role in several areas of health, including skin health, female hormonal health and children’s health
References
- Shahidi F, Ambigaipalan P. Omega-3 Polyunsaturated Fatty Acids and Their Health Benefits. Annu Rev Food Sci Technol. 2018 Mar 25;9:345-381. doi: 10.1146/annurev-food-111317-095850. PMID: 29350557.
- Djuricic I, Calder PC. Beneficial Outcomes of Omega-6 and Omega-3 Polyunsaturated Fatty Acids on Human Health: An Update for 2021. Nutrients. 2021 Jul 15;13(7):2421. doi: 10.3390/nu13072421. PMID: 34371930; PMCID: PMC8308533.
- Sergeant S, Rahbar E, Chilton FH. Gamma-linolenic acid, Dihommo-gamma linolenic, Eicosanoids and Inflammatory Processes. Eur J Pharmacol. 2016 Aug 15;785:77-86. doi: 10.1016/j.ejphar.2016.04.020. Epub 2016 Apr 12. PMID: 27083549; PMCID: PMC4975646.
- Simopoulos AP. An Increase in the Omega-6/Omega-3 Fatty Acid Ratio Increases the Risk for Obesity. Nutrients. 2016 Mar 2;8(3):128. doi: 10.3390/nu8030128. PMID: 26950145; PMCID: PMC4808858.
- Zhang Y, Sun Y, Yu Q, Song S, Brenna JT, Shen Y, Ye K. Higher ratio of plasma omega-6/omega-3 fatty acids is associated with greater risk of all-cause, cancer, and cardiovascular mortality: A population-based cohort study in UK Biobank. Elife. 2024 Apr 5;12:RP90132. doi: 10.7554/eLife.90132. PMID: 38578269; PMCID: PMC10997328.
- DiNicolantonio JJ, O’Keefe J. The Importance of Maintaining a Low Omega-6/Omega-3 Ratio for Reducing the Risk of Autoimmune Diseases, Asthma, and Allergies. Mo Med. 2021 Sep-Oct;118(5):453-459. PMID: 34658440; PMCID: PMC8504498.
- Mercola J, D’Adamo CR. Linoleic Acid: A Narrative Review of the Effects of Increased Intake in the Standard American Diet and Associations with Chronic Disease. Nutrients. 2023 Jul 13;15(14):3129. doi: 10.3390/nu15143129. PMID: 37513547; PMCID: PMC10386285.
- Mariamenatu AH, Abdu EM. Overconsumption of Omega-6 Polyunsaturated Fatty Acids (PUFAs) versus Deficiency of Omega-3 PUFAs in Modern-Day Diets: The Disturbing Factor for Their “Balanced Antagonistic Metabolic Functions” in the Human Body. J Lipids. 2021 Mar 17;2021:8848161. doi: 10.1155/2021/8848161. PMID: 33815845; PMCID: PMC7990530.
- Sharifi M, Nourani N, Sanaie S, Hamedeyazdan S. The effect of Oenothera biennis (Evening primrose) oil on inflammatory diseases: a systematic review of clinical trials. BMC Complement Med Ther. 2024 Feb 15;24(1):89. doi: 10.1186/s12906-024-04378-5. PMID: 38360611; PMCID: PMC10867995.
- da Costa Hime LFC, Carvalho Lopes CM, Roa CL, Zuchelo LTS, Baracat EC, de Andrade J, Soares JM Jr. Is there a beneficial effect of gamma-linolenic acid supplementation on body fat in postmenopausal hypertensive women? A prospective randomized double-blind placebo-controlled trial. Menopause. 2021 Feb 1;28(6):699-705. doi: 10.1097/GME.0000000000001740. PMID: 33534427.
- D’Helft J, Caccialanza R, Derbyshire E, Maes M. Relevance of ω-6 GLA Added to ω-3 PUFAs Supplements for ADHD: A Narrative Review. Nutrients. 2022 Aug 10;14(16):3273. doi: 10.3390/nu14163273. PMID: 36014778; PMCID: PMC9416383.
- D’Helft J, Caccialanza R, Derbyshire E, Maes M. Relevance of ω-6 GLA Added to ω-3 PUFAs Supplements for ADHD: A Narrative Review. Nutrients. 2022 Aug 10;14(16):3273. doi: 10.3390/nu14163273. PMID: 36014778; PMCID: PMC9416383.
- Mustonen AM, Nieminen P. Dihomo-γ-Linolenic Acid (20:3n-6)-Metabolism, Derivatives, and Potential Significance in Chronic Inflammation. Int J Mol Sci. 2023 Jan 20;24(3):2116. doi: 10.3390/ijms24032116. PMID: 36768438; PMCID: PMC9916522.
- Niseteo T, Hojsak I, Ožanić Bulić S, Pustišek N. Effect of Omega-3 Polyunsaturated Fatty Acid Supplementation on Clinical Outcome of Atopic Dermatitis in Children. Nutrients. 2024 Aug 24;16(17):2829. doi: 10.3390/nu16172829. PMID: 39275147; PMCID: PMC11397185.
- Won JC, Kwon HS, Moon SS, Chun SW, Kim CH, Park IB, Kim IJ, Lee J, Cha BY, Park TS. γ-Linolenic Acid versus α-Lipoic Acid for Treating Painful Diabetic Neuropathy in Adults: A 12-Week, Double-Placebo, Randomized, Noninferiority Trial. Diabetes Metab J. 2020 Aug;44(4):542-554. doi: 10.4093/dmj.2019.0099. Epub 2019 Nov 4. PMID: 31701699; PMCID: PMC7453980.
- Sharifi M, Nourani N, Sanaie S, Hamedeyazdan S. The effect of Oenothera biennis (Evening primrose) oil on inflammatory diseases: a systematic review of clinical trials. BMC Complement Med Ther. 2024 Feb 15;24(1):89. doi: 10.1186/s12906-024-04378-5. PMID: 38360611; PMCID: PMC10867995.
- Veselinovic M, Vasiljevic D, Vucic V, Arsic A, Petrovic S, Tomic-Lucic A, Savic M, Zivanovic S, Stojic V, Jakovljevic V. Clinical Benefits of n-3 PUFA and ɤ-Linolenic Acid in Patients with Rheumatoid Arthritis. Nutrients. 2017 Mar 25;9(4):325. doi: 10.3390/nu9040325. PMID: 28346333; PMCID: PMC5409664.
- Simon D, Eng PA, Borelli S, Kägi R, Zimmermann C, Zahner C, Drewe J, Hess L, Ferrari G, Lautenschlager S, Wüthrich B, Schmid-Grendelmeier P. Gamma-linolenic acid levels correlate with clinical efficacy of evening primrose oil in patients with atopic dermatitis. Adv Ther. 2014 Feb;31(2):180-8. doi: 10.1007/s12325-014-0093-0. Epub 2014 Jan 17. PMID: 24435467; PMCID: PMC3930832.
- Chung BY, Park SY, Jung MJ, Kim HO, Park CW. Effect of Evening Primrose Oil on Korean Patients With Mild Atopic Dermatitis: A Randomized, Double-Blinded, Placebo-Controlled Clinical Study. Ann Dermatol. 2018 Aug;30(4):409-416. doi: 10.5021/ad.2018.30.4.409. Epub 2018 Jun 27. PMID: 30065580; PMCID: PMC6029968.
- Olejnik A, Gornowicz-Porowska J, Jenerowicz D, Polańska A, Dobrzyńska M, Przysławski J, Sansone A, Ferreri C. Fatty Acids Profile and the Relevance of Membranes as the Target of Nutrition-Based Strategies in Atopic Dermatitis: A Narrative Review. Nutrients. 2023 Sep 4;15(17):3857. doi: 10.3390/nu15173857. PMID: 37686888; PMCID: PMC10489657.
- Muggli R. Systemic evening primrose oil improves the biophysical skin parameters of healthy adults. Int J Cosmet Sci. 2005 Aug;27(4):243-9. doi: 10.1111/j.1467-2494.2005.00274.x. PMID: 18492193.
- Balić A, Vlašić D, Žužul K, Marinović B, Bukvić Mokos Z. Omega-3 Versus Omega-6 Polyunsaturated Fatty Acids in the Prevention and Treatment of Inflammatory Skin Diseases. Int J Mol Sci. 2020 Jan 23;21(3):741. doi: 10.3390/ijms21030741. PMID: 31979308; PMCID: PMC7037798.
- Jung JY, Kwon HH, Hong JS, Yoon JY, Park MS, Jang MY, Suh DH. Effect of dietary supplementation with omega-3 fatty acid and gamma-linolenic acid on acne vulgaris: a randomised, double-blind, controlled trial. Acta Derm Venereol. 2014 Sep;94(5):521-5. doi: 10.2340/00015555-1802. PMID: 24553997.
- Mahboubi M. Evening Primrose (Oenothera biennis) Oil in Management of Female Ailments. J Menopausal Med. 2019 Aug;25(2):74-82. doi: 10.6118/jmm.18190. Epub 2019 Aug 5. PMID: 31497576; PMCID: PMC6718646.
- Kumari J, Amrita, Sinha A, Kumari S, Biswas P, Poonam. Effectiveness of Evening Primrose and Vitamin E for Cyclical Mastalgia: A Prospective Study. Cureus. 2024 Apr 11;16(4):e58055. doi: 10.7759/cureus.58055. PMID: 38752050; PMCID: PMC11095819.
- Safdari F, Motaghi Dastenaei B, Kheiri S, Karimiankakolaki Z. Effect of Evening Primrose Oil on Postmenopausal Psychological Symptoms: A Triple-Blind Randomized Clinical Trial. J Menopausal Med. 2021 Aug;27(2):58-65. doi: 10.6118/jmm.21010. PMID: 34463069; PMCID: PMC8408320.
- Ghavi F, Shakeri F, Farahnaz H, Abdolahian S. Comparison of the Effect of Fennel and Evening Primrose Oil on Menopausal Problems and Hormonal Levels: A Randomized Controlled Trial. Iran J Nurs Midwifery Res. 2023 Jul 24;28(4):430-435. doi: 10.4103/ijnmr.ijnmr_149_22. PMID: 37694196; PMCID: PMC10484391.
- Mehrpooya M, Rabiee S, Larki-Harchegani A, Fallahian AM, Moradi A, Ataei S, Javad MT. A comparative study on the effect of “black cohosh” and “evening primrose oil” on menopausal hot flashes. J Educ Health Promot. 2018 Mar 1;7:36. doi: 10.4103/jehp.jehp_81_17. PMID: 29619387; PMCID: PMC5868221.
All of our blogs are written by our team of expert Nutritional Therapists. If you have questions regarding the topics that have been raised, or any other health matters, please do contact them using the details below:
nutrition@cytoplan.co.uk
01684 310099
Find out what makes Cytoplan different
Last updated on 5th February 2025 by cytoffice



Very informative findings, backed up by evidence from studies, which I found interesting to read so I can take action to look at my diet and supplement intake. Thank you
Hello,
Thank you for your feedback, it’s great to hear that you find the blog posts so interesting.