This in-depth and highly researched article by Eshani King, a researcher in immunology and health, follows on from her first piece for us; ‘The role of vitamin D and COVID-19 – the latest research‘.
This review adopts an integrated, comprehensive approach in reviewing the emerging evidence and developments from varying sources to consolidate and add to the knowledge base on vitamin D and Covid-19. Highlighting the central role of vitamin D deficiency in Covid-19 pathology mediated by an uncontrolled excess of angiotensin II and bradykinin, as well as the failure of T-cells, it builds on evidence previously reviewed in May 2020 on the role of vitamin D deficiency in Covid-19 deaths [1].
Accumulating evidence to date points strongly to vitamin D deficiency being a causal factor in the serious pathology seen with Covid-19, rather than just a contributory one. This means a paradigm shift in our perception of the role of vitamin D from being one of many potential interventions to a major causal factor in serious illness, hospitalisation, and death. In people who do not have compromised immune systems, Covid-19 is usually a relatively mild illness and evidence suggests it becomes serious only when the immune system lacks sufficient vitamin D, or when the viral load is excessively high. Some 150 scientists, doctors and leading authorities wrote an open letter on 7 December 2020 calling for immediate widespread action by governments worldwide to increase vitamin D use to combat Covid-19 [2]. These signatories each note their recommendation for supplementation together with their own personal daily supplementation levels. It is noteworthy that the vast majority recommend 4,000 IU (10 times the level recommended in the UK), but many take amounts in excess of this, of up to 10,000 IU.
It is also notable that last May, the French National Academy of Medicine recommended rapid vitamin D testing for all over 60s diagnosed with COVID-19, with immediate administration of a high bolus dose of 50,000-100,000 IU if they are found to be deficient, and daily supplementation with 800-1000 IU for everyone else [3]. Last June, the Academy of Medical Scientists and Professor of Immunology at Imperial College, Charles Bangham, urged ministers to bolster public health messages on vitamin D. Recently, the positive attention vitamin D has received, for example in the article “Vitamin D and Covid-19 Evidence and Recommendations for Supplementation” published in the Royal Society’s Open Science is to be welcomed [4]. It proposes a doubling of the current recommended intake to 800 IU, which although a positive step, is still too low. More recently, MP David Davis made a convincing case for vitamin D in Parliament on 14 January, speaking with considerable knowledge on the matter [5]. The response from Jo Churchill, the Parliamentary Under-Secretary of State for Health and Social Care, was, however, non-committal.
- “Vitamin” D is unique and is mis-named a “vitamin”
It is unfortunate that Vitamin D was mis-named as this gives the impression that it is just another vitamin; it is not a vitamin (vital amine) but a fundamentally important steroid hormone responsible for the epigenetic control (switching on and off) of genes. Every human cell has vitamin D receptors (VDR) for binding vitamin D and 2,776 binding sites have been identified for VDR in human DNA [6]. It is also unfortunate that, while the role of vitamin D in bone health is repeatedly emphasised in discussions on the topic, its central and vital role in immunity is often not given sufficient prominence, even though VDRs control at least 300 genes involved in immunity to infection and to cancer [7]. Uniquely, unlike every other nutrient, food is only a minor source of vitamin D. Throughout evolution, humans have relied on the action of sunlight on the skin to make vitamin D from a cholesterol derivative but at UK latitudes, above the 35th parallel where UVB radiation is weak, virtually no vitamin D is made between September and April or outside 10am to 3 pm even in summer months. Darker skinned individuals in the UK make very little vitamin D even between 10am and 3pm in the summer as melanin pigment in the skin blocks UV light [8]. As humans moved away from the equator, those who lost the melanin pigment in their skin and became paler skinned had an evolutionary advantage which enabled them to continue making sufficient vitamin D in latitudes with less UV light. This process continued, with increasingly paler skin enabling further northward migration.
Food and water are not the only essentials for human survival; we were designed by evolution to require sunlight, not only to make vitamin D but, as emerging evidence indicates, to derive a multitude of other benefits from it. As just one of many examples, parts of the infra-red spectrum elevate levels of Brain-derived Neurotrophic Factor, enhancing neuronal growth and improving mental health [9].
2. The UK population has some of the lowest levels of vitamin D
The UK is located at a higher latitude than is generally appreciated. At 50°N -60°N, it is further North than the US and at a similar latitude to Southern Canada [10]. UK average levels of vitamin D have been found to be below 20 ng/ml (50 mmol/l) [11] which is considered by vitamin D experts around the world to be a deficient level for immunity, with Scotland having the highest levels of deficiency in the UK [10]. A serum level 30 ng/ml (75 mmol/l) is considered sufficient, while optimum immunity is thought to require levels above 40ng/ml (100 mmol/l) [12]. Vitamin D is a fat-soluble hormone: in the UK, in the early part of the 20th century, diets were higher in vitamin D rich animal fats, butter, cream, offal, and fatty fish which provided some vitamin D even in winter months and cod liver oil was a valued supplement. Food fortification with vitamin D was common between 1930 and 1950 [13]. Interestingly, during that period, no new strains of flu were recorded and there were no pandemics. However, UK levels have plummeted in the last 40-50 years or so. Whist reliable older data is difficult to find for the UK, a study from the US indicates that levels started falling sharply from the 1970s to the late 1990s [14]. The decline coincided with the “health” drive against saturated fats and the wide acceptance of the now increasingly challenged cholesterol heart hypothesis. It also coincided with the beginning of the widespread use of sun cream which can block up to 95% of vitamin D production [8,15].
An August 2020 study using UK Biobank data from over 6,400 people of Indian, Pakistani, or Bangladeshi background found that an astounding 92% had vitamin D levels of less than 20 ng/ml, a level deficient for immunity, with 55% having less than 10 ng/ml (25 mmol/l), indicating extreme deficiency [16].
A substantial recent Australian-funded study of almost 416,000 UK Biobank participants led by Professor Hypponen, found what the researchers described as an “alarming” prevalence of vitamin D deficiency in the UK” [17] as shown on the graph at fig 1. It can be readily seen that even in the summer, less than a third of people achieve levels consistent with sufficient immunity of above 30 ng/ml (or 75 nmol/l), and that the mean (from the dotted line using the axis on the right in mmol/l) remains well below a mere 24 ng/l (or 60 nmol/l). By January, only a very tiny proportion achieves sufficient levels. The proportion of the population with levels above 40 ng/ml (or 100 mmol/l) was not separately reported.
When the results were further analysed, Asians in the UK were, surprisingly, found to be even more deficient in vitamin D than those of Black African heritage. In winter, 57.2% of Asian, 38.5% of Black African, 36.5% of mixed, 33.1% of Chinese and 17.5% of White European heritage were severely deficient in vitamin D for the purposes of immunity with levels at or below 10 ng/ml (or 25 nmol/l). The figure of 55% for the percentage of Asians with levels below 10 ng/ml from the previously mentioned August study is very close to the 57.2% derived from this recent study. Unfortunately, there are no other numbers that are directly comparable as the data for the proportions of each group with levels of vitamin D below 20 ng/ml (below which levels are considered deficient for immunity) were not established in the later study. These are certain to be far higher and possibly in line with findings in the August study.
Low levels of vitamin D have long been known to increase susceptibility to respiratory viruses and are also strongly implicated in cardiovascular disease, hypertension, skin conditions (including psoriasis), autoimmunity (including MS, lupus, ulcerative-colitis, and type 1 diabetes), neurological conditions, cancers (including those of the breast and prostate) and many other serious health conditions [1,12]. Furthermore, in addition to previously observed increases in risk of some of these conditions for the offspring of vitamin D deficient mothers [18], a more recent finding of concern is that lower vitamin D levels in the second trimester of pregnancy is associated with a lower IQ of the child at age 4-6 [19].
Unacceptably low UK levels of vitamin D should be considered a national emergency which needs to be rectified by immediate, decisive action.
3. Trial design, quality of evidence and the critical importance of magnesium
A review of the evidence for vitamin D in preventing or reducing Covid-19 was carried out by NICE (the National Institute for Health and Care Excellence) in June 2020 [20]. However, it is very narrow in scope, limiting itself to examining 5 studies which it considers to be the best available evidence. This concluded that insufficient evidence existed from Randomised Controlled Trials (RCTs) that vitamin D can help with Covid-19. As detailed in a critical analysis of the NICE report [21], the evidence used could have been interpreted in exactly the opposite way if the following issues had been considered in greater depth: adjustment for confounders insisted on by NICE were arguably, inappropriate; the Scientific Advisory Committee on Nutrition (SANC) review that NICE relied upon included studies that used either too low a vitamin D dose to make any difference or an extremely high potentially toxic one-off bolus dose; very old data was used; and there were major fundamental omissions of relevant factors. These omission include a significant body of established biochemical and immunological evidence that were simply ignored.
In the past, some RCTs on vitamin D intervention for various conditions have, unfortunately, been carried out without the proper detailed biological understanding necessary for their correct design, with the inevitable consequence that they do not show a benefit for vitamin D intervention. In particular, there is evidence that most western populations are deficient in magnesium [22]. Magnesium is involved in both of the steps in the hydroxylation of vitamin D, initially to 25-hydroxyvitamin D, the form detected by most serum vitamin D tests, and the second hydroxylation to 1,25-dihydroxyvitamin D, the most active form. Magnesium is also required for the binding of vitamin D to its transport protein, Vitamin D Binding Protein, without which it cannot travel in the bloodstream to the kidneys and to all the cells involved in immunity where, crucially, the second hydroxylation takes place [22]. Magnesium deficiency is thus a limiting factor which can prevent a vitamin D intervention from raising serum levels of vitamin D despite a plentiful intake of vitamin D. As magnesium deficiency is extremely common, all vitamin D intervention studies should also supplement with magnesium and have a third arm to tease out the separate effects of magnesium alone. It should also be noted that magnesium deficiency cannot be measured by looking at serum levels (apparently the only measurement currently generally available through the NHS); as magnesium is of critical importance to over 700 biochemical reactions in the body, serum levels are tightly regulated and maintained within a very narrow range, if necessary, by pulling magnesium out of tissues. Even in a state of gross magnesium deficiency, serum levels will be maintained until the situation becomes an emergency. A red blood cell measurement is a better indicator of deficiency and although not perfect, may be used as a proxy measurement of magnesium levels [22]. It is a great pity that the issue of magnesium is not considered in many otherwise well-designed trials. An alternative strategy is to bypass one of the magnesium dependent steps and use the once hydroxylated form, 25-hydroxyvitamin D, otherwise known as calcifediol. If a patient in an intervention study is already critically ill, this alternative would enable vitamin D to act in a matter of hours rather than the several days or weeks it would normally require for the conversion to occur in the liver.
Reverting to NICE‘s June review, one Swiss study examined by NICE, carried out by D ’Avolio [22] is highly significant in that it answers a different question not asked in any other COVID-19 study – although this particular aspect of it was not commented on by NICE. The study examined out-patients who came into a hospital with similar symptoms of respiratory illness to be tested for Covid-19. It found that out-patients that were confirmed as COVID-19 positive had significantly lower levels of vitamin D than out-patients with very similar symptoms of respiratory illness but who were COVID-19 negative. Quoting from the previous review [1], an analysis of the immunology and biochemistry involved in a SARS-type infection at section 5 led to the suggestion that “ Given the descriptions in this section, the strength of response of the innate immune system’s first line defence system, which is highly dependent on vitamin D status, is potentially of far greater importance than in a non-SARS, non-COVID-19 respiratory infection….”. The findings in D’Avolio demonstrate this premise, i.e., that higher levels of vitamin D appear to be needed for combatting Covid-19 infections than for most other viral infections.
In virtually every case, a vitamin D study that has arrived at a negative result has, on further detailed investigation, been found to have had serious design flaws, for example, inappropriate dosage of vitamin D as illustrated in the detailed examination of studies used in the SANC review [21], inappropriate comparisons, or where the intervention is made too late. It is unfortunate that many meta-analyses carried out over the years of vitamin D studies also do not filter out all such studies, with the result that they report very modest benefits for vitamin D. More recent examples are two very similar Mendelian randomisation studies comparing people who have genetic variations which predispose them to have differing levels of vitamin D [24,25]. Both studies found that those people with genetically determined higher levels of vitamin D had an increased risk of disease. However, the comparison between groups with differing genetic variations is not a meaningful comparisons; there are very likely to be other compensatory differences in biochemistry associated with these hereditary genetic differences which are too complex to identify and tease out, especially as these might sometimes occur at mitochondrial level. It is difficult to understand why these comparisons were deemed appropriate for determining efficacy of vitamin D.
Finally, NICE stated that it would like to see larger RCTs before it can accept that vitamin D is helpful. It is interesting that, as early as June 2019, a novel artificial intelligence aided method pioneered by Dr Gareth Davies and associates, termed Causal Inference Analysis provided very high-quality evidence that “vitamin D plays a causal role in Covid-19 outcomes” explicitly without need for further RCTs. The authors note that:
“The size and scope of available data used in our analysis is unprecedented with almost 240 global reporting locations with 1.6 million confirmed infections and covering a population of circa 1 billion, making it potentially one of the highest power causal inference studies ever performed. Using a hypothetico-deductive method, 100% of testable predictions verified the causal model and falsified the acausal model, providing compelling evidence in favour of a causal relationship in advance of RCTs. The application of observational causal inference methods is relatively new in medicine, but their many advantages in time, cost, study size and strength of evidence suggests they should rank higher in the hierarchy of evidence and play a major role in the future of medical research” [13].
The paper contains an excellent well-reasoned analysis of the relative merits of different types of scientific evidence which should be of great interest to all reviewers of scientific literature including members of NICE. It challenges the prevailing orthodoxy that RCTs should always take precedence over observational studies and explains that inflexible fixation with RCTs is often misplaced; RCTs can often be of poor quality and participants are often not representative of the population while conversely, observational studies can often be high quality, highly powered and supported by strong biological evidence.
It is of significance that for vitamin D, despite the lack of industry funding, we now have excellent evidence derived from every type of study, as examined in the following pages.
4. RCTs, observational and correlation studies
Our understanding of the role of vitamin D in Covid-19 cases and deaths has progressed considerably since the previous review of May 2020 [1]. To recap briefly, in addition to numerous early correlation and observational studies supporting a role for vitamin D, a relatively small (n=212) but very interesting study from the Philippines reported that severe cases of Covid-19 are associated with low vitamin D levels. This was followed in April by Indonesian research using data from a larger group of 780 hospitalised patients who had tested positive for COVID-19 [26]: while only 4% of patients with sufficient levels of vitamin D >30ng/ml (OH)D, died, the mortality rate was 87.8% and 98.9% in the insufficient (20-30ng/ml), and deficient (<20ng/ml), groups, respectively.
Evidence has continued to accumulate and the case for vitamin D has grown ever more compelling. In addition to the Causal Inference Analysis already discussed at section 3, there have been further large-scale correlation studies, small RCTs and hundreds of other studies from around the world. A few of the more significant or interesting of these have been selected for further examination or mention.
A Spanish study found that 82% of 216 patients admitted to hospital with Covid-19 were deficient in vitamin D, compared to only 47% in a population-based control group [27]. After adjusting for confounders, an Iranian study of 235 hospital patients found a significant association between vitamin D sufficiency and reduction in clinical severity and mortality and levels of C-reactive protein (CRP), an indicator for inflammation. Only 9% of vitamin D sufficient patients with levels above 30 ng/ml died compared to 20% of patients with levels below 30 ng/ml [ 28].
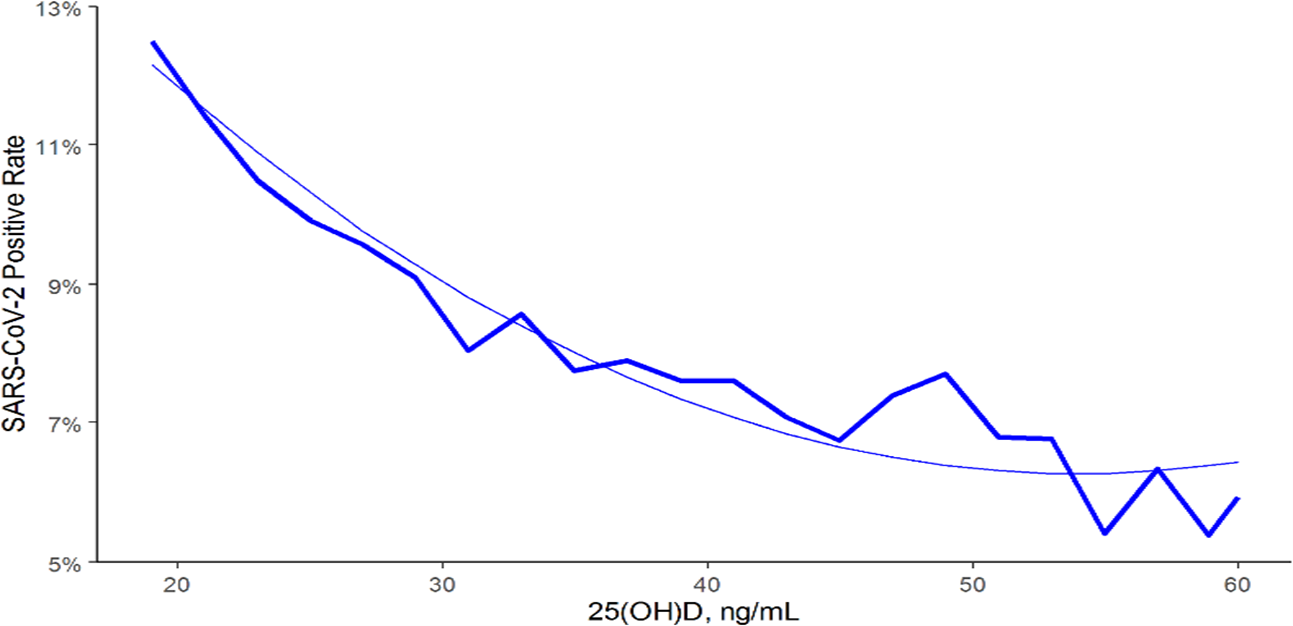
A substantial and highly convincing observational study led by Professor Holick of Boston University included almost 200,000 people [29]. The overall results shown at fig 2 unambiguously illustrate that the higher the prior recorded vitamin D level taken from medical records, the lower the chances of testing positive. This strong consistent relationship was seen within each separate data set for over and under age 60, male v female, latitude (northern, central, and southern), and race (black, Hispanic, and white). Within every subgroup, the data clearly shows that the higher the vitamin D levels, the less likely an individual is to be diagnosed as Covid-19 positive. The authors state that “there is a strong and intense association between circulating 25(OH) vitamin D and levels of SARS-CoV-2 positivity”. This study overcomes previous questioning of the Filipino and Indonesian studies on the basis that perhaps it was the severity of the illness that led to the low vitamin D levels rather than low vitamin D levels causing the severity of illness. It should be noted that even if this Boston study and further studies described below had never been carried out, it is clear that logically, whichever way round the causality, additional vitamin D must be required; it must either or both be used up during illness so that additional supplies are needed and/or, it is used to defend against illness, in which case additional supplies are still needed.
In this trial, the hydroxylated form of vitamin D, calcifediol or 25-hydroxyvitamin D, was used. As already described, this circumvents the need for magnesium sufficiency and the intervention also takes far less time to take effect and it is therefore highly appropriate as a treatment when time is critical. Despite dismissal from NICE with suggestions that this was not a truly double-blind study, that there were methodological issues and that the sample size was too small (which meant the results for deaths is not statistically significant), there can be no disputing that the ICU result, even given the size of the sample, was statistically highly significant. Deaths, of course, cannot be influenced by blinding and therefore NICE’s reservations could be regarded as unfounded.
These question marks may have lingered had not scientific rigour come to the rescue in the form of scientists at the Massachusetts Institute of Technology (MIT) who considered it a worthwhile investment of their time to analyse the study in depth. As noted by David Grimes, a former gastroenterologist and vitamin D researcher/author: “The MIT analysis is one of great detail, and it puts to shame the cursory approach of NICE. It researched the conduct of the study as well as analysing its results. The conclusion is that there was no fault in the conduct of the Córdoba trial. It acknowledged that the findings are robust, and that the chance of the results being in error is less than 1 in 60,000” [31]. The MIT analysis [32] itself concludes very robustly:
“Here we reanalyse the results of the study using rigorous and well-established statistical techniques, and find that the randomization, large effect size, and high statistical significance address many of these concerns. In particular, we show that decreased ICU admissions were not due to uneven distribution of comorbidities or other prognostic indicators, to imperfect blinding, or to chance, but were instead associated with the calcifediol intervention. We conclude that the Córdoba study provides sufficient evidence to warrant immediate, well-designed pivotal clinical trials of calcifediol in a broader cohort of inpatients and outpatients with COVID-19, and to consider broad adoption of calcifediol treatment for vitamin-D-deficient hospitalized COVID-19 patients.”
This high dose calcifediol trial was expanded and continued in 5 hospitals. It was concluded recently, and the paper is currently undergoing peer review with the results eagerly awaited. Also expected later this year are the results from a UK RCT led by Professor Martineau of the Queen Mary University of London. This trial compares two doses of vitamin D, 800 IU or 3,200 IU to a placebo group to assess whether vitamin D can help in the prevention of illness.
Another small RCT from India looked at patients who were admitted with Covid-19 with low Vitamin D levels but excluded those who were seriously ill [33].
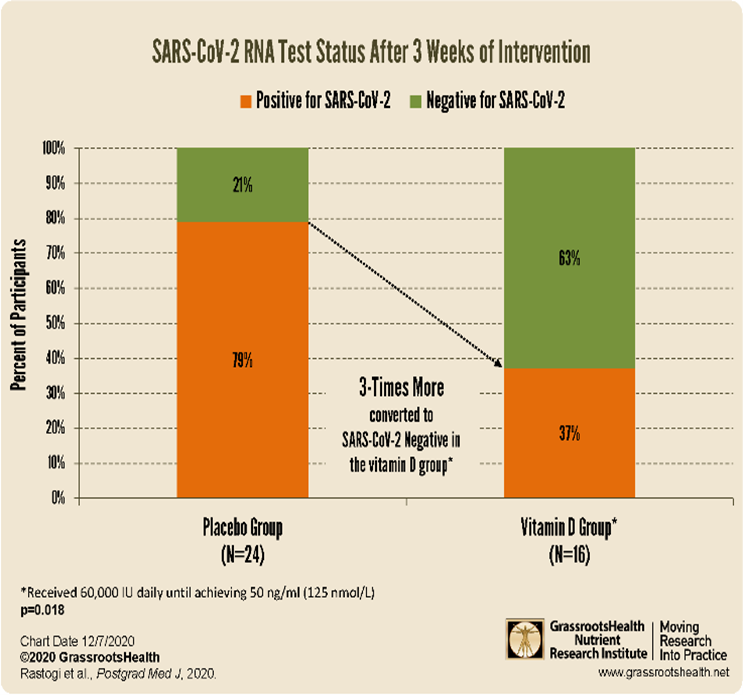
16 were allocated to a high dose vitamin D group which had average starting vitamin D levels of only 8.6 ng/ml (21.5 nmol/l) and 24 to a placebo group with average levels of only 9.5 ng/ml/ (23.7 nmol/l). Of the 16 patients receiving 60,000 IU of vitamin D per day, 10 increased their vitamin D levels to at least 50 ng/ml after 7 days of supplementing, and another two required continued supplementation to reach 50 ng/ml by day 14. By the end of 3 weeks, three times more, or 63% of patients in the vitamin D group became SARS-CoV-2 negative, compared to only 21% of the 24 patients in the control group (p=0.018). Vitamin D intervention was therefore shown to help clear a Covid-19 infection faster in such mild to moderate cases.
Despite receiving 60,000 IU of vitamin D for 7-14 days there was no indication of toxicity in the vitamin D group. It is a pity that the severely ill group was excluded from this trial.
A very large Israeli study of almost 1.4 million people by Ben-Gurion University found a significant negative correlations between prior recorded vitamin D levels taken from medical records and the risk of testing positive for Covid-19 [34]. This strong association was consistently seen in different ethnic groups and males and females separately. The effect was especially pronounced in Arab women who are traditionally covered up and spend more time indoors, i.e., these women were highly deficient in vitamin D and had correspondingly significantly higher rates of infection. The results suggested that the risk of death from Covid-19 could be halved in some groups by vitamin D optimisation and that liquid vitamin D supplementation, but not a tablet formulation, was associated with lower Covid-19 incidence. It is also interesting that Israel suffered far fewer Covid-19 related deaths than neighbouring Iran which sits at a similar latitude. The population of Iran, being largely Arab and covered up, have far lower vitamin D levels [35].
Finally, a newly released highly significant study finally answers the long-standing question about seasonality of respiratory viruses [36]. There has been much protracted debate over the years about the underlying reason for seasonality, with opposing views citing humidity, heat, or UV light/vitamin D levels. A mathematical examination of the timing of the winter surge in Covid-19 infections in 18 European countries finally proved there is no correlation with humidity, temperature or with school opening dates. Instead, an “impressive” linear correlation of the timing of the surge was found with latitude, and in particular, the precise time at which the UV daily dose dropped to 34% of the strength at 0° latitude, regardless of lockdowns or restrictions. The ability of humans to make vitamin D and/or the ability of UV light to kill viruses now remain as the only two viable reasons for seasonal resurgence of viruses.
5. Biological evidence
5.1 Background: As the pathology of Covid-19 has gradually become better understood, the detailed biochemical/immunological evidence for the role of vitamin D deficiency has become increasingly convincing. Existing research had already established that vitamin D acts epigenetically to switch on genes that increase human antiviral (cathelicidin LL37 and defensins) production, strengthen first line physical defences such as tight junctions and mucosal linings, mobilise and increase various types of immune cells, reduce blood clotting and coagulation, and modulate the adaptive immune system to prevent it tipping into overdrive and autoimmunity [1, section 5]. The following findings, particularly important in Covid-19 pathology, cement the central role of vitamin D deficiency in the progression of illness.
5.2 Cytokine and bradykinin “storms”: Angiotensin-converting enzyme 2 (ACE2) is a metallomonocarboxypeptidase enzyme located in membranes and highly expressed in lung tissue, particularly in type II pneumocytes, ciliated cells, transient secretory cells and also in the smooth muscle of blood vessels, the heart, intestines, and kidneys. It is part of the renin-angiotensin (RAS) system which regulates the cardiovascular system and kidneys [37-39]. ACE2 is also part of the kinin-kallikrein system (KKS) which controls blood pressure, vascular permeability, and influences blood clotting [40,41]. Angiotensin Converting Enzyme (ACE) and ACE2 balance each other’s actions. ACE converts angiotensin I to angiotensin II which initiates highly complex inflammatory cascades leading to inflammation. ACE2 dampens this by degrading angiotensin II to angiotensin 1-7 (by cleaving a single C-terminal residue) which mediates anti-inflammatory pathways. When uncontrolled, excess angiotensin II can lead to ARDS (acute respiratory distress syndrome), lung inflammation, lung injury, alveolar epithelial cell apoptosis and coagulatory effects [38,39,42].
ACE2 also controls excess bradykinin (BK) which is now thought by many researchers to be responsible for much of the more unusual pathology observed in severe Covid-19 cases [40-46] initiated by signalling of des-Arg9 bradykinin (DABK), the active metabolite of BK, through bradykinin B1 receptor, BKB1R [43,44]. This induces neutrophil infiltration via chemokines which contributes significantly to the pathology of pulmonary inflammatory disorders, lung damage and mortality. The signalling pathways also result in vascular permeability and leakage via vasodilation of arterioles and vasoconstriction of venules and capillaries, leading to low blood pressure and the other more unusual pathology observed in severe Covid-19. Examples of these are “Covid-19 toes”, “Covid tongue” allodynia (nerve irritation and pain) and hyperalgesia (hypersensitivity to pain). BK sensitizes somatosensory fibres via a chemical cascade which includes release of nitric oxide, prostacyclin, prostaglandin 1 and endothelial derived hyperpolarising factor or EDHF. Excess BK can also be the cause of a dry cough as indeed also seen in many patients on ACE inhibitor drugs [43]. It is also associated with hypokalaemia (low potassium), connected with arrythmia and sudden cardiac death, both of which are reported in Covid-19. Crucially, ACE2 controls the effects of excessive DABK by degrading it and prevents the varied symptoms and pathology described [43,44].
SARS-CoV-2 causes derangement of both the RAS and the KKS because ACE2 is internalised by binding of SARS-CoV-2 spike glycoprotein. This prevents it from performing the two important degrading steps of angiotensin II and DABK described above. Vitamin D, however, upregulates genes for VDR and ACE2, making additional functional ACE2 available to enzymatically cleave angiotensin II and DABK and so restores balance, dampening down inflammation and preventing build-up of both angiotensin II and active DABK, [46,47]. The increased VDR blocks transcription of renin which is part of the RAS and required to convert angiotensinogen to angiotensin I, thus reducing further the levels of the substrate available for conversion into angiotensin II [46,47].
Some researchers have commented that African Americans have an increased sensitivity to the effects of BK, and this was thought to be caused by a specific genetic difference connected to angioedema [43]. However, it is also possible that this heightened sensitivity could be caused by a higher level of vitamin D deficiency. It is also interesting to note here that the rate of degradation of BK is generally higher for women than for men [45].
A research team used the US Department of Energy’s Oak Ridge National Laboratory’s Summit supercomputer, currently the US’s most powerful supercomputer, to analyse genes in lung cell fluid from Covid-19 patients, the results attracting much attention from commentators. The beginning of the abstract of the paper, first published in July 2020 states: “ Neither the disease mechanism nor treatments for Covid-19 are currently known. Here we present a novel molecular mechanism for Covid-19 that provides therapeutic intervention points that can be addressed with existing FDA approved pharmaceuticals”. The team found that BK gene expression is, indeed, excessively switched on, and expression of the VDR reduced [48]. This is in line with the descriptions above. However, they also found that ACE2 expression was upregulated which does not, at first, appear to make a great deal of sense. If there had indeed been plenty of functional ACE2, as they apparently found, then active BK (i.e., DABK, the active metabolite), would be rapidly degraded leaving little to cause the serious pathology observed in Covid-19.
At this stage, it is important to appreciate a limitations of any findings that are based upon gene expression; upregulation of genes does not necessarily indicate a corresponding increase in the actual protein into which the RNA is translated. This is because not all RNA will necessarily be translated and also because proteins may be degraded or altered immediately following translation. Therefore, great caution is required in interpreting the results of these types of studies.
It has been observed that interferons and viruses induce upregulation of what looks very much like ACE2 when detected by methods such as 3’-scRNA-seq and gene-based assays. However, research from July 2020 demonstrates that the type of ACE2 induced by interferons and viruses, including specifically by SARS-CoV-2, is a different isoform of ACE2, named by the researchers, delta-ACE2 or dACE2, which shares common gene sequences with ACE2 and therefore likely to be misidentified by gene-based assays. This isoform was found to be incapable of acting as an entry point for SARS-CoV2. In addition, it lacks the normal enzymatic functions described earlier as it lacks 356 N-terminal amino acids, thus rendering it ineffective as a binding site for SARS-Cov-2, or as a carboxypeptidase which cleaves a C-terminal residue from both angiotensin II and DABK [49]. Although the view of the researchers is that dACE2 it is very likely to have an important function, what this might be is currently unknown. What is almost certain, therefore, is that the Oak Ridge researchers were detecting, not functional ACE2, but its isoform, dACE2.
In a highly detailed paper elaborating on the biochemical interactions involved, the researchers note that BK is degraded by ACE but omit the step in which the active metabolite of BK, DABK, is degraded by ACE2. There is simply no mention of DABK in the paper, which is puzzling. This major omission and the question mark about the upregulation of ACE2 means that the various interactions and causal relationships the model proposes cannot fit together. This is presumably why the model does not agree with that proposed by van de Veerdonk and many others [40,41], a difference that the Oak Ridge team appear to be aware of and mention in their paper. It is interesting that Frank van de Veerdonk himself was a peer reviewer of the Oak Ridge paper. It might be assumed that neither party was, at the time, aware of the research identifying the isoform, published at around the same time in July in pre-print, but this does not explain the omission of DABK from their considerations and their model.
The team went on to consider what interventions would be effective in reducing BK levels. In their table of potential interventions, vitamin D appears at position 5 after a number of drugs such as Icatiband and Danazol. This was based solely on the effect of vitamin D in downregulating the gene for renin. However, as the researchers omitted the active metabolite of BK, DABK, and established research showing that this is degraded by ACE2, they also missed the significance of functional ACE2 expression (as opposed to the isoform) being upregulated by vitamin D, as described earlier. As functional ACE2 is upregulated by vitamin D, the ability to control levels of both DABK and angiotensin II can be restored by vitamin D. This alone merits the immediate promotion of vitamin D from 5th place, directly to the number one position on the table of interventions that can dampen a BK storm.
Indeed, numerous researchers have proposed that drugs that can increase ACE2, or alternatively, the use of artificial recombinant ACE2 might be effective treatments in SARS type infections and some of these suggestions are currently being trialled.
5.3 T-cells have been shown to be crucial: The ability to mount a strong innate and T-cell response is likely to result in a mild case. Research from Yale University and elsewhere shows that in mild or asymptomatic cases, many CD4+ and CD8+ T-cells are generated at an early stage and that these are highly varied, responding not just to parts of the Spike (S) protein or Receptor Binding Domain but to many other parts of the virus. Notably, in these mild cases there were few or no detectable antibodies. Conversely, the severely ill produced few T-cells with less variety but they had plenty of antibodies [50-53]. This demonstrates that a strong early T-cell response can successfully control the virus, preventing progression of illness. On a first exposure, antibody production generally takes 7-14 or more days and is of increased importance in the event that the innate and T-cell responses are unable to prevent disease progression.
Existing research has already established that T-cells will simply not activate without sufficient vitamin D. As the lead researcher, head of the Department of International Health, Immunology and Microbiology at the University of Copenhagen, Carsten Geisler, noted many years ago: “When a T cell is exposed to a foreign pathogen, it extends a signalling device or ‘antenna’ known as a vitamin D receptor, with which it searches for vitamin D,” and if there is an inadequate vitamin D level, “they won’t even begin to mobilize” [54]. The question of whether T-cells might also need a continuing supply of vitamin D to prevent the T-cell exhaustion and apoptosis observed in some serious Covid-19 cases deserves further research.
There is evidence from various sources which point to an important role for T-cells in protective pre-existing immunity to Covid-19 derived from prior encounters with other coronaviruses [1,55].
5.4 Other symptoms, hypoxia, anosmia: Excessive hyaluronic acid (HA) production has been proposed in the Oak Ridge study as a potentially important factor in the accumulation of fluid in the lungs and upregulation of the gene for HA synthesis was seen in severe cases [48]. HA can trap 1000 times its weight in water to form a hydrogel similar to that found in the bronchoalveolar spaces of the lungs of severely ill patients. When combined with vascular permeability caused by BK, the viscous hydrogel reduces the surface area available for gas exchange drastically, thus causing hypoxia or lack of oxygen. Pushing more oxygen into the lungs will, therefore, be of limited help; indeed, ventilation of such patients has proved to be counterproductive and hyperbaric oxygen considered the more appropriate treatment. HA has also been associated with the pulmonary thrombosis and/or ground glass opacities seen in Covid-19 in radiological findings [48]. There is evidence that the gene regulating hyaluronic acid production is downregulated by vitamin D and the gene regulating its breakdown, upregulated [55].
Anosmia (loss of the sense of smell) is a symptom that can be explained by vitamin D and/or zinc deficiency. This sensory loss has also been reported in patients with hereditary angioedema and in persons taking ACE inhibitors [43]. Anosmia can also be caused by the infection depleting zinc reserves; zinc deficiency has long been associated with anosmia from flu and other viral infections [57]. Zinc is known to inhibit reverse transcriptase and thereby prevent viral replication: this may provide one explanation for its depletion in the course of many viral infections. Zinc also acts on the KKS described above to reduce BK levels by inhibiting the kallikrein protease enzyme responsible for converting kinins to BK [48]. Often in mild Covid-19, the only symptom is anosmia, and it might be that this occurs in people who have sufficient vitamin D but have low zinc reserves.
5.5 Blood Clotting: Additional evidence that vitamin D reduces blood clotting comes from findings that it drastically reduces platelet aggregation in type 1 diabetes [57]. Mitochondria of platelets are rich in VDR and as platelets are anuclear, this must act either non-genomically, perhaps through the regulation of calcium flows, or through control of mitochondrial DNA [58].
5.6 Long Covid : Long lasting symptoms such as fatigue, breathlessness, anxiety and depression, palpitations, joint or muscle pain and ‘brain fog’ following a viral illness have long been recognised and are not uncommon. These post viral fatigue syndromes have, at various times, been given many names including Chronic Fatigue Syndrome (CFS), Myalgic Encephalomyelitis (ME) and Yuppy Flu. Every one of these symptoms is also typical of vitamin D deficiency and therefore it is quite possible that depletion of vitamin D reserves during infection is the underlying cause. If this theory is correct, symptoms should be alleviated by administering vitamin D. A Vitamin D trial to test this hypothesis would be very welcome. Chest pains and other lingering symptoms could also be the result of lasting damage caused by cytokine and BK storms which may need significant time to heal and this, as shown above, could also indicate that vitamin D levels were insufficient during the illness.
6. Integrating evidence from other sources
We all recall the frightening footage from Wuhan and Northern Italy that caused worldwide panic. These are two areas of the world worst affected by atmospheric pollution which completely blocks UVB of 290-310nm needed to make vitamin D. People in these two areas would be expected to be highly vitamin D deficient, as indeed found to be the case: 76% of Italian women between 60-80 years had vitamin D levels below 12 ng/ml and 82% had levels below 5 ng/ml in patients on long term rehabilitation programmes, while the mean level in the Wuhan population was only 13ng/ml (32.5 nmol/l) [60-62], far lower levels than seen even in the UK population. These images are engraved in our minds, but the far emptier hospital wards elsewhere in the world where there are better vitamin D levels, including the rest of China, Africa, Singapore, and many other hot sunny Asian countries, were naturally, of little interest to the media. Japan was infected early, clearly reaching a high percentage (at least 50%) of the population as demonstrated by repeated antibody tests, and despite a high population density, no lockdowns, and the oldest population on the planet, it escaped with very few deaths [63]. Japan also has the highest vitamin D levels found in elderly populations anywhere, largely due to a traditional fish rich diet [64]. Covid-19 seems to be a relatively mild illness in people who have serum levels of vitamin D similar to those found in indigenous people such as the Maasai and Hadzabi, of 40-60 ng/ml [12,65]. These appear to be the levels that evolution and biology have designed us to operate with.
It is interesting that the realisation that dark-skinned populations living in the west are more prone to infectious diseases is not at all a recent one. This has been known for well over 250 years; in a book on history and politics, published in London in 1760, William Douglas MA wrote : “The small-pox in cold countries is more fatal to blacks than whites. In Boston smallpox of 1752, there died whites in the natural way about one in eleven…..;blacks in the natural way one in eight…” [66]. In stark contrast, Nigeria with its population of 200 million has seen very few COVID-19 deaths or serious cases. According to Nigerian press reports, a doctor and Special Advisor to the former President has written at length to attribute this to sunshine and high vitamin D levels [67]. There must be at least as much poverty and nutritional deprivation (and very likely far more) in Nigeria as there is in the UK or the US where far more black people have died of COVID-19. It therefore becomes difficult to sustain the argument that excess deaths of black people in the UK and USA are largely down to poverty, deprivation, and poor nutrition. In this context, the following information and graph at fig 4 from Dr D Grimes, are of interest. The graph shows the age of all doctors who died from Covid-19 in the UK whose obituaries appeared in the British Medical Journal, by broad ethnicity [68]. Although 13 BAME doctors were included, there were a further 10 who did not have their obituaries in the BMJ, making the total number of BME doctors who died of Covid-19 between 25 March and 3 May 23. In that period only 1 white working doctor died from Covid-19 which means that 96% of working doctors who died were of BAME origin. Only one of the white doctors was working and so the rest shown in the graph were presumably retired. The comparison is very interesting as it compares one group of doctors with another who have a roughly similar socio-economic status. It is difficult to argue there was any poverty, deprivation or any other factor involved other than the colour of their skin. It is very clear that while the white retired doctors and one working doctor died at a normal age, all the doctors of BAME origin died well before their time, some up to 30 years before. It is striking that there is no overlap in the ages of death. Although it may be argued that doctors of BAME origin may generally have more co-morbidities than their white counterparts, it should be recognised that these co-morbidities could themselves well be the result of sustained vitamin D deficiency [1,12]. After all, in addition to the Nigerian example above, poor people living in Indian slums but with plenty of access to sunlight also have an incredibly low death rate from Covid-19.

It is also striking that the deaths came to a very abrupt end on 3 May with the end of the spring pandemic and there has only been one further death from Covid-19 in 2020, that of a doctor of BAME origin, in November. The reason may be that levels of sunshine and vitamin D started to rise, and that in the resurgence starting in September, doctors had already been exposed to Covid-19 and were largely immune. It may be that the vitamin D message has got through to BAME doctors; a letter advising vitamin D supplementation was sent to hospital doctors in April. Or perhaps there are other factors, or a combination of these.
The evidence discussed above taken together indicates that serious Covid-19 pathology is often the result of an immune system that is dysregulated because of the lack of vitamin D, the epigenetic master controller required for it to function optimally and in a measured, regulated manner. Of course, this is not to say there are no other reasons for becoming susceptible to Covid-19: only that there are many very strong evidence-based reasons to conclude that correcting vitamin D deficiency is highly likely to reduce the numbers of deaths and hospitalisations from Covid-19 significantly.
7. Concerns surrounding toxicity
7.1 General: The current guidance suggests vitamin D levels above 4,000 IU may be toxic. However, over 20,000 IU of vitamin D equivalent can be produced in 30 minutes by a Caucasian from full sun exposure in summer in the UK and it is therefore highly implausible that 4,000 IU (or indeed 20,000 IU) can be toxic [15]. The European Food Safety Panel’s Statement of Scientific Opinion, EFSA 28 Oct 2016, acknowledges that no adverse effects have been observed at 10,000 IU or 250 mcg per day. True vitamin D toxicity is actually extremely rare in the medical literature and has never been demonstrated at daily doses below 50,000 IU [15,69]. For context, lifeguards are known to maintain blood levels of above 100ng/ml (or 250 mmol/l) without ill effects, over 5 times the average level for the UK population of less that 20 ng/ml (or 50 mmol/l) [11]. It should be borne in mind that, as highlighted at section 3, the aim of vitamin D supplementation is to correct a state of serious and widespread Vitamin D deficiency that has largely arisen from plummeting levels in the last 30-50 years. How can correcting a deficiency lead to toxicity? Vitamin D deficiency itself is a recognised significant threat to health and we should be far more concerned about this than about unsubstantiated claims regarding toxicity.
7.2 Excess calcium and other nutrients: What is occasionally mistaken for vitamin D toxicity is the effect of excess calcium caused by the increase in calcium absorption mediated by vitamin D [69]. This can very occasionally be a problem in people with rare conditions or compromised kidney function if very high amounts of vitamin D are taken, but doctors should be able to identify anyone with such a risk. The more recent common practice of calcium supplementation to attempt to reduce osteoporosis risk could be a real issue in this respect. Additional calcium is likely to be both unnecessary and undesirable when there is adequate vitamin D as vitamin D increases calcium absorption from the gut. Vitamin K2 activates matrix GLA protein and osteocalcin, two calcium binding proteins which have the effect of removing excess calcium from arteries and depositing it in bones, hence also leading to an additional benefit of lower blood pressure [70]. If calcium toxicity is a concern, supplementing with vitamin K2 is advisable as a precaution in case normal intake of vitamin K2 from food sources is inadequate. Some vitamin D supplements already include K2.
8. Appropriate dose
8.1 General: The current recommended level of 400 IU, a level that was based many years ago on the intake required for bone health and also on the amount contained in a teaspoon of cod liver oil, is far too low for optimum immunity. Research has shown that 400 IU daily is not capable of raising serum levels of vitamin D above even 10ng/ml (or 25 mmol/l) which is the threshold for being severely deficient for the purposes of immunity [71].
A serum vitamin D level of 40 ng/ml (or 100 nmol/l) is the generally accepted minimum level for optimum immunity. “The Big Vitamin D Mistake”, a paper uncovering statistical errors in previous work, shows that a previous study found that 8895 IU per day is needed for 97.5% of individuals to achieve blood levels equal to or above 20 ng/ml (50 nmol/l), whilst another study had found 9122 IU/d was required to achieve 40 ng/ml (100nmol/l). It also notes that “the largest meta-analysis ever conducted of studies published between 1996 and 2013 showed that 25 Hydroxyvitamin D levels of <75 nmol/l [equivalent to 30 ng/ml] may be too low for safety and associated with higher all-cause mortality….”. [72].
The US administration’s infectious disease expert, Dr Fauci, has confirmed he takes 6,000 IU daily [73]. Based on the information provided, it is likely that most people probably need between 6,000 and 10,000 IU from all sources, including food and sun, to maintain serum levels at 40 ng/ml or above. Therefore, assuming there is some limited intake from food, the recommended supplementation levels from Autumn to Spring should be increased to 4,000 – 8,000 IU daily from September to April, supported by relatively inexpensive serum vitamin D testing to assess serum levels so that appropriate adjustments may be made to the intake. People with darker skin will need to supplement even in summer although at a slightly lower level. Further guidance on supplementation levels are available in a separate article [74]. Research shows that regular rather than bolus dosing is important, and it should be noted that levels take several weeks to increase from a low baseline [4]. A UV lamp of the correct wavelength and strength is another alternative that could be considered, particularly for care homes.
D2 from vegetable sources has been found to be less effective at being converted to the active form than D3 from animal sources [75]. Vitamin D is fat soluble and commonly available in capsule form using an oil-based carrier. Compressed solid tablets may be of limited effectiveness as they are less bio-available; in common with other fat-soluble vitamins such as vitamin A, E and K, fat is required in order to absorb vitamin D. In summer, when vitamin D can be made in the skin, less supplementation is needed, but sunscreen, full clothing, wide-brimmed hats, beards, and masks all reduce the available skin surface area for making it. The dose required is roughly proportional to body size.
8.2. Magnesium: As discussed, magnesium is required to hydroxylate vitamin D and therefore, deficiency of magnesium can be an important limiting factor even in vitamin D sufficient individuals. Magnesium deficiency is extremely widespread in western countries and is a particular problem amongst the very active, individuals under chronic stress, people on medications and those consuming high levels of carbohydrates/grains/sugars. In all these instances, magnesium becomes significantly depleted. For these reasons, combined with dietary changes over the decades and severe soil depletion of magnesium, it is very difficult to sustain adequate magnesium levels from food alone [22,76,77]. Magnesium supplementation and reduction of sugar/carbohydrates from the diet to raise magnesium levels is highly recommended alongside vitamin D supplementation.
A note on Vitamin D and adverse reactions from vaccination
It is possible that people who are most at risk of suffering serious illness from Covid-19 are also the most likely to suffer adverse reactions from vaccination. The immune modulatory effects of vitamin D in the adaptive immune system have been discussed in the May 2020 review already referred to [1]. Based on the immunological mechanisms involved, it is possible that vitamin D deficiency has the potential to increase the risk of adverse reactions to vaccinations as the normal mechanisms to prevent over-reaction of the immune system and autoimmunity are dampened. Studies are urgently required to establish whether this might be the case. That said, a well and fully functioning immune system can provide robust protection and the case for vaccination of a person who has optimal levels of vitamin D is therefore less compelling. Vaccination will also further deplete vitamin D levels as the immune system will mount a reaction in a similar (though not the same) way as it will to the actual virus and therefore, vitamin D sufficiency is advisable prior to vaccination.
Conclusion
In addition to correlation studies, we now have very solid evidence from scientific research, not only that serious Covid-19 cases and deaths are strongly associated with vitamin D deficiency, but that the higher a person’s vitamin D status, the lower the chances of contracting Covid-19. In addition, intervention studies have confirmed that administering vitamin D, particularly in the form of calcifediol, to hospitalised patients, reduces the need for ICU significantly, reduces deaths and clears the virus more rapidly. Research from the last 7 months has added considerably to the existing substantial body of evidence demonstrating a very strong case for biological plausibility.
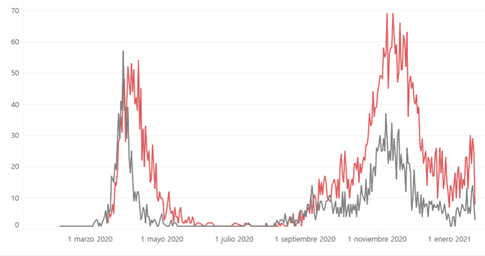
The Andalusian regional governing body discussed the existing research on 6 November 2020 and concluded that sufficient evidence existed to recommend vitamin D in the form of calcifediol to be distributed to care homes and to be dispensed to patients by doctors [78]. It is notable that within a matter of a few weeks, from the beginning of December, hospitalisations and deaths fell sharply, reversing the usual annual trend, so that by the beginning of January daily deaths had dropped from round 60 to around 10 [79]. It appears to have risen since before falling back down. It is unclear exactly how much calcifediol was dispensed, how long this was sustained for and to what extent the recommendations were followed, but something certainly appears to have triggered this dramatic downturn. It could not have been vaccination as the vaccination programme in Andalusia started on 27 December 2020.
It is hoped that the UK will be able to learn from this experience. What is certainly clear is that individuals supplementing with the low daily dose of 10mcg or 400 IU, as currently recommended by the UK Government, are destined to remain in a highly deficient state which renders them susceptible to infections of all types, including with SARS-CoV-2. It also increases the rate of serious illness and death from multiple other causes. A 2007 study reports that vitamin D supplement use was far lower in the UK (13% of men and 20% of women), than in the US (30% of men and 40% of women) and vitamin D intake through food was half of that in the US [10].
Certain sections of the public are already aware of the need to take far higher doses outside the summer months and many experts have been critical of government inaction on raising the recommended levels. Unlike informed members of the public, the most deprived sections of the population who are most in need of it are less likely to be in a position to help themselves. Taking urgent action to significantly increase the recommended supplementation levels, to provide oil-based vitamin D supplements of appropriate strength and vitamin D tests to people on low incomes, particularly those of BAME origin, as well as to care homes through the NHS, should be a national priority. The evidence calls for the government to also launch a strong and sustained publicity campaign to promote vitamin D as a cheap, very safe, and highly effective health intervention which will save lives and significantly improve general health; as many commentators have already noted, there is little to lose and much to gain.
Postscript: Further to the small pilot calcifediol study from Cordoba, a second, much larger trial with 930 Covid-19 patients at Hospital Del Mar, Barcelona recently confirmed the spectacular results obtained with calcifediol intervention: a greater than 80% reduction in the need for ICU and a greater than 50% reduction in mortality (after adjusting for age, gender, serum vitamin D levels at baseline, and comorbidities). It was also confirmed that higher baseline vitamin D levels are associated with a reduced risk of needing ICU and a reduced risk of death. This was not a double blind RCT but rather an open RCT. Although there are a few aspects of the trial which have attracted unfounded critisism from detractors, these are wholly defendable, and it is difficult to argue that the effects are not both real and highly significant. This should have provided the icing on an already substantial cake.
Unfortunately, this paper has now been withdrawn under pressure from external sources for reasons that appear spurious. A Brazilian study which has many serious faults ( using a bolus dose, giving it far too late, and providing it in a form that takes at least a week or two to convert to a form useful for the immune system in even well people, etc.) has instead breezed through the peer review process to be rapidly published. This study, as I’m sure you might have guessed by now, didn’t show that vitamin D helped significantly. This seems to be the sad state of vitamin D research at the moment but even more worryingly, the hijacking of science extends far beyond vitamin D.
Key Takeaways
- Accumulating evidence to date points strongly to vitamin D deficiency being a causal factor in the serious pathology seen with Covid-19
- Food and water are not the only essentials for human survival; we were designed by evolution to require sunlight, not only to make vitamin D but, as emerging evidence indicates, to derive a multitude of other benefits from it
- Food fortification with vitamin D was common between 1930 and 1950 [13]. Interestingly, during that period, no new strains of flu were recorded and there were no pandemics. However, UK levels have plummeted in the last 40-50 years or so
- A mathematical examination of the timing of the winter surge in Covid-19 infections in 18 European countries finally proved there is no correlation with humidity, temperature or with school opening dates. Instead, an “impressive” linear correlation of the timing of the surge was found with latitude, and in particular, the precise time at which the UV daily dose dropped to 34% of the strength at 0° latitude, regardless of lockdowns or restrictions. The ability of humans to make vitamin D and/or the ability of UV light to kill viruses now remain as the only two viable reasons for seasonal resurgence of viruses.
- Existing research has already established that T-cells will simply not activate without sufficient vitamin D
- Long COVID: Long lasting symptoms such as fatigue, breathlessness, anxiety and depression, palpitations, joint or muscle pain and ‘brain fog’ following a viral illness have long been recognised and are not uncommon. Chest pains and other lingering symptoms could also be the result of lasting damage caused by cytokine and BK storms which may need significant time to heal and this could also indicate that vitamin D levels were insufficient during the illness
- Covid-19 seems to be a relatively mild illness in people who have serum levels of vitamin D similar to those found in indigenous people such as the Maasai and Hadzabi, of 40-60 ng/ml. These appear to be the levels that evolution and biology have designed us to operate with
- The realisation that dark-skinned populations living in the west are more prone to infectious diseases is not at all a recent one. This has been known for well over 250 years
- The evidence discussed above taken together indicates that serious Covid-19 pathology is often the result of an immune system that is dysregulated because of the lack of vitamin D, the epigenetic master controller required for it to function optimally and in a measured, regulated manner. Of course, this is not to say there are no other reasons for becoming susceptible to Covid-19: only that there are many very strong evidence-based reasons to conclude that correcting vitamin D deficiency is highly likely to reduce the numbers of deaths and hospitalisations from Covid-19 significantly
- Magnesium is required to hydroxylate vitamin D and therefore, deficiency of magnesium can be an important limiting factor even in vitamin D sufficient individuals. Magnesium deficiency is extremely widespread in western countries and is a particular problem amongst the very active, individuals under chronic stress, people on medications and those consuming high levels of carbohydrates/grains/sugars
- Based on the immunological mechanisms involved, it is possible that vitamin D deficiency has the potential to increase the risk of adverse reactions to vaccinations as the normal mechanisms to prevent over-reaction of the immune system and autoimmunity are dampened. Studies are urgently required to establish whether this might be the case
- In addition to correlation studies, we now have very solid evidence from scientific research, not only that serious Covid-19 cases and deaths are strongly associated with vitamin D deficiency, but that the higher a person’s vitamin D status, the lower the chances of contracting Covid-19
About the author
Eshani King BSc (Hons) Biochemistry, FCA, CTA, BFP
Evidence Based Research in Immunology and Health
Eshani has been passionate about science from a very early age. Following a degree in Biochemistry with an option in immunology at Bristol University, Eshani changed direction and qualified as a Chartered Accountant with KPMG, specialising in corporate taxation. In 1998 Eshani left her accountancy career in order to devote time to carrying out research to help alleviate the serious health issues that one of her close family members developed.
As a member of the BAME community with family members who potentially have a high risk from a COVID-19 infection, she was highly motivated to examine existing and recent research supporting the role of vitamin D deficiency in COVID-19 outcomes.
With many thanks to Eshani King for this highly researched and in-depth article. If you have questions regarding the topics that have been raised, or any other health matters, please do contact me (Amanda) by phone or email at any time.
amanda@cytoplan.co.uk
01684 310099
Amanda Williams and the Cytoplan Editorial Team
References:
- King, E. 2020. “The Role of Vitamin D Deficiency in COVID-19 Related Deaths in BAME, Obese and Other High-risk Categories.” NutriXiv. June 17. https://doi.org/10.31232/osf.io/73whx
- Over 100 Scientists, Doctors, & Leading Authorities Call for IncreasedVitamin D Use to Combat COVID-19: Scientific evidence indicates vitamin D reduces infections & deathshttps://vitamind4all.org/letter.html
- Academie Nationale de Medicine. Vitamin D and Covid-19 Press release from the French National Academy of Medicine 22 May 2020 https://www.academie-medecine.fr/wp-content/uploads/2020/05/20.5.22-Vitamine-D-et-coronavirus-ENG.pdf
- George Griffin et al. Vitamin D and COVID-19: evidence and recommendations for supplementation. R. Soc. open sci.7201912. 1 Dec 20 http://doi.org/10.1098/rsos.201912
- Vitamin D:Covid-19. Volume 687: Debated Thursday 14 January 2021 https://hansard.parliament.uk/Commons/2021-01-14/debates/32A497CB-0B5D-4C8B-9974-AB02678ADA3B/details
- Ramagopalan SV, Heger A, Berlanga AJ, et al. A ChIP-seq defined genome-wide map of vitamin D receptor binding: associations with disease and evolution. Genome Research. 2010 Oct;20(10):1352-1360. DOI: 10.1101/gr.107920.110 .
- Hossein-nezhad A, Spira A, Holick MF. Influence of vitamin D status and vitamin D3 supplementation on genome wide expression of white blood cells: a randomized double-blind clinical trial. PLoS One. 2013;8(3):e58725. doi:10.1371/journal.pone.0058725
- Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80(6 Suppl):1678S‐88S. doi:10.1093/ajcn/80.6.1678S
- Low-Level Laser Therapy Rescues Dendrite Atrophy via Upregulating BDNF Expression: Implications for Alzheimer’s Disease. Chengbo Meng, Zhiyong He, Da Xing. Journal of Neuroscience 14 August 2013, 33 (33) 13505-13517; DOI: 10.1523/JNEUROSCI.0918-13.2013
- Hyppönen E, Power C. Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr. 2007 Mar;85(3):860-8. doi: 10.1093/ajcn/85.3.860. PMID: 17344510.
- Lips, Paul et al (2019). MANAGEMENT OF ENDOCRINE DISEASE: Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency; a position statement of the European Calcified Tissue Society. European Journal of Endocrinology. 180. 10.1530/EJE-18-0736
- Charoenngam N, Holick MF. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients. 2020 Jul 15;12(7):2097. doi: 10.3390/nu12072097. PMID: 32679784; PMCID: PMC7400911.
- Gareth Davies, Attila R Garami, Joanna Byers. Evidence Supports a Causal Role for Vitamin D Status in Global COVID-19 Outcomes. medRxiv 2020.05.01.20087965; doi: https://jdoi.org/10.1101/2020.05.01.20087965
- O’Brien D.M., Thummel K.E., Bulkow L.R., Wang Z., Corbin B., Klejka J., Hopkins S.E.,Singleton R. Declines in traditional marine food intake and vitamin D levels from the 1960s to present in young Alaska Native women (2017) Public Health Nutrition, 20 (10) , pp. 1738-1745. https://doi.org/10.1017/S1368980016001853
- Holick MF. Vitamin D: a d-lightful solution for health. J Investig Med. 2011 Aug;59(6):872-80. doi: 10.2310/JIM.0b013e318214ea2d. PMID: 21415774; PMCID: PMC3738435.
- Darling AL, Blackbourn DJ, Ahmadi KR, Lanham-New SA. Very high prevalence of 25-hydroxyvitamin D deficiency in 6433 UK South Asian adults: analysis of the UK Biobank Cohort. Br J Nutr. 2020 Jul 22:1-12. doi: 10.1017/S0007114520002779. Epub ahead of print. PMID: 32693845.
- Sutherland JP, Zhou A, Leach MJ, Hyppönen E. Differences and determinants of vitamin D deficiency among UK biobank participants: A cross-ethnic and socioeconomic study. Clin Nutr. 2020 Nov 25:S0261-5614(20)30639-7. doi: 10.1016/j.clnu.2020.11.019. Epub ahead of print. PMID: 33309415.
- Hypponen, E; Boucher, BJ; (2010) Avoidance of vitamin D deficiency in pregnancy in the United Kingdom: the case for a unified approach in National policy. BRIT J NUTR , 104 (3) 309 – 314. 1017/S0007114510002436.
- Melough MM, Murphy LE, Graff JC, Derefinko KJ, LeWinn KZ, Bush NR, Enquobahrie DA, Loftus CT, Kocak M, Sathyanarayana S, Tylavsky FA. Maternal Plasma 25-Hydroxyvitamin D during Gestation Is Positively Associated with Neurocognitive Development in Offspring at Age 4-6 Years. J Nutr. 2020 Nov 2:nxaa309. doi: 10.1093/jn/nxaa309. Epub ahead of print. PMID: 33136167.
- NICE: Vitamin D for Covid-19. Evidence Review. https://www.nice.org.uk/advice/es28/evidence/evidence-review-pdf-8777674477
- King. Critical Analysis of NICE review of vitamin D for Covid-19. 17 June 2020 https://drive.google.com/file/d/1AHDn7MhNTaxQhuEj1j0Rfga1waLZa_UP/view?usp=drivesdk
- Anne Marie Uwitonze, BDT, MS; Mohammed S. Razzaque, MBBS, PhD Role of Magnesium in Vitamin D Activation and Function . February 2018; The Journal of the American Osteopathic Association 118(3) doi:https://doi.org/10.7556/jaoa.2018.037
- Antonio D’Avolio et al. 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2. 9 May 20. Nutrients 2020, 12(5), 1359; https://doi.org/10.3390/nu12051359
- J Brent Richards Vitamin D and Covid-19 Susceptibility and Severity: a Mendelian Randomization 1 Study https://doi.org/10.1101/2020.09.08.20190975doi: medRxiv preprint posted September 10, 2020.
- Amin HA, Drenos F. No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data. BMJ Nutrition, Prevention & Health 2021;bmjnph-2020-000151. doi: 10.1136/bmjnph-2020-000151
- Raharusun, Prabowo and Priambada, Sadiah and Budiarti, Cahni and Agung, Erdie and Budi, Cipta, Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study (April 26, 2020 updated 6 May). Available at SSRN: https://ssrn.com/abstract=3585561 or http://dx.doi.org/10.2139/ssrn.3585561
- Hernández JL, Nan D, Fernandez-Ayala M, García-Unzueta M, Hernández-Hernández MA, López-Hoyos M, Muñoz-Cacho P, Olmos JM, Gutiérrez-Cuadra M, Ruiz-Cubillán JJ, Crespo J, Martínez-Taboada VM. Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection. J Clin Endocrinol Metab. 2020 Oct 27:dgaa733. doi: 10.1210/clinem/dgaa733. Epub ahead of print. PMID: 33159440.
- Z, Holick. M. et al, Vitamin D Sufficiency Reduced Risk for Morbidity and Mortality in COVID-19 Patients (5/27/2020). Available at SSRN: https://ssrn.com/abstract=3616008 or http://dx.doi.org/10.2139/ssrn.3616008
- Kaufman HW, Niles JK, Kroll MH, Bi C, Holick MF (2020) SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLOS ONE 15(9): e0239252. https://doi.org/10.1371/journal.pone.0239252
- Marta Entrenas Castillo et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. The Journal of Steroid Biochemistry and Molecular Biology. Volume 203, October 2020, 105751. https://doi.org/10.1016/j.jsbmb.2020.105751
- David grimes blog: Covid-19 19 and Vitamin D. Calcifediol – Report from Massachusetts Institute of Technology. http://www.drdavidgrimes.com/2020/11/
- Irwin Jungreis, Manolis Kellis Mathematical analysis of Córdoba calcifediol trial suggests strong role for Vitamin D in reducing ICU admissions of hospitalized COVID-19 patients.
medRxiv 2020.11.08.20222638; doi: https://doi.org/10.1101/2020.11.08.20222638
- Rastogi A, Bhansali A, Khare N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study).Postgraduate Medical Journal Published Online First: 12 November 2020. doi: 10.1136/postgradmedj-2020-139065
- Ariel Israel MD, PhD. The link between vitamin D deficiency and Covid-19 in a large population. medRxiv preprint. September 7,2020 https://doi.org/10.1101/2020.09.04.20188268doi
- Tabrizi R, Moosazadeh M, Akbari M, Dabbaghmanesh MH, Mohamadkhani M, Asemi Z, et al. High Prevalence of Vitamin D Deficiency among Iranian Population: A Systematic Review and Meta-Analysis. Iran J Med Sci. 2018;43: 125. Available: https://www.ncbi.nlm.nih.govui/pmc/articles/PMC5936844/
- Walrand, S. Autumn COVID-19 surge dates in Europe correlated to latitudes, not to temperature-humidity, pointing to vitamin D as contributing factor. Sci Rep 11, 1981 (2021). https://doi.org/10.1038/s41598-021-81419-w
- Re, R.N. Mechanisms of disease: local renin-angiotensin-aldosterone systems and the pathogenesis and treatment of cardiovascular disease. Nat Clin Pract Cardiovasc Med1, 42-7 (2004)
- Santos, R.A. Angiotensin-(1-7). Hypertension63, 1138-47 (2014).
- Diamond, B. The renin-angiotensin system: An integrated view of lung disease and coagulopathy in COVID-19 and therapeutic implications. J Exp Med217(2020)
- van de Veerdonk, F.L.et al.Kallikrein-kinin blockade in patients with COVID-19 to prevent acute respiratory distress syndrome. Elife9(2020).
- de Maat, S., de Mast, Q., Danser, A.H.J., van de Veerdonk, F.L. & Maas, C. Impaired Breakdown of Bradykinin and Its Metabolites as a Possible Cause for Pulmonary Edema in COVID-19 Infection. Semin Thromb Hemost(2020).
- Mahmudpour M, Roozbeh J, Keshavarz M, Farrokhi S, Nabipour I. COVID-19 cytokine storm: The anger of inflammation. Cytokine. 2020 Sep;133:155151. doi: 10.1016/j.cyto.2020.155151. Epub 2020 May 30. PMID: 32544563; PMCID: PMC7260598.
- Roche, JA, Roche, R. A hypothesized role for dysregulated bradykinin signaling in COVID-19‐19 respiratory complications. The FASEB Journal. 2020; 34: 7265– 7269. https://doi.org/10.1096/fj.202000967
- Chinder P. Sodhi, et al Attenuation of pulmonary ACE2 activity impairs inactivation of des-Arg9 bradykinin/BKB1R axis and facilitates LPS-induced neutrophil infiltration .American Journal of Physiology-Lung Cellular and Molecular Physiology 2018 314:1, L17-L31
- Cyr M, Lepage Y, Blais C Jr, Gervais N, Cugno M, Rouleau JL, Adam A. Bradykinin and des-Arg(9)-bradykinin metabolic pathways and kinetics of activation of human plasma. Am J Physiol Heart Circ Physiol. 2001 Jul;281(1):H275-83. doi: 10.1152/ajpheart.2001.281.1.H275. PMID: 11406494.
- Xu J, Yang J, Chen J, Luo Q, Zhang Q, Zhang H. Vitamin D alleviates lipopolysaccharide‑induced acute lung injury via regulation of the renin‑angiotensin system. Mol Med Rep. 2017;16(5):7432‐7438. doi:10.3892/mmr.2017.7546
- Yang, Jelena & Zhang, Hanxiao & Xu, Jianjian. (2016). Effect of Vitamin D on ACE2 and Vitamin D receptor expression in rats with LPS-induced acute lung injury. 25. 1284-1289. 10.3760/cma.j.issn.1671-0282.2016.12.016.
- Garvin MR, Alvarez C, Miller JI, Prates ET, Walker AM, Amos BK, Mast AE, Justice A, Aronow B, Jacobson D. A mechanistic model and therapeutic interventions for COVID-19 involving a RAS-mediated bradykinin storm. Elife. 2020 Jul 7;9:e59177. doi: 10.7554/eLife.59177. PMID: 32633718; PMCID: PMC7410499.
- Onabajo OO, Banday AR, Stanifer ML, Yan W, Obajemu A, Santer DM, Florez-Vargas O, Piontkivska H, Vargas JM, Ring TJ, Kee C, Doldan P, Tyrrell DL, Mendoza JL, Boulant S, Prokunina-Olsson L. Interferons and viruses induce a novel truncated ACE2 isoform and not the full-length SARS-CoV-2 receptor. Nat Genet. 2020 Dec;52(12):1283-1293. doi: 10.1038/s41588-020-00731-9. Epub 2020 Oct 19. PMID: 33077916.
- Annika Nelde, Tatjana Bilich, Jonas S. Heitmann et al. SARS-CoV-2 T-cell epitopes define heterologous and COVID-19-induced T-cell recognition, 16 June 2020, Research Square https://www.researchsquare.com/article/rs-35331/v1%20
- Avraham Unterman, et al. Single-Cell Omics Reveals Dyssynchrony of the Innate and Adaptive Immune System in Progressive COVID-19. medRxiv 2020.07.16.20153437; doi: https://doi.org/10.1101/2020.07.16.20153437
- Leticia Kuri-Cervantes, et al. Immunologic perturbations in severe COVID-19/SARS-CoV-2 infection. bioRxiv 2020.05.18.101717; doi: https://doi.org/10.1101/2020.05.18.101717
- Floriane Gallais, et al. Intrafamilial Exposure to SARS-CoV-2 Induces Cellular Immune Response without Seroconversion. medRxiv 2020.06.21.20132449; doi: https://doi.org/10.1101/2020.06.21.20132449
- Von Essen MR, Kongsbak M, Schjerling P, Olgaard K, Odum N, Geisler C. Vitamin D controls T cell antigen receptor signaling and activation of human T cells. Nat Immunol. 2010;11(4):344-349. doi:10.1038/ni.1851
- King response to BMJ. T-cells really are the superstars in fighting COVID-19 – but why are some of us so poor at making them? 21 September 2020:
https://www.bmj.com/content/370/bmj.m3563/rr-6
- Carmen J. Narvaez, Seamus Balinth, JoEllen Welsh. Vitamin D inhibits hyaluronan synthesis and extracellular matrix gene expression in triple negative breast cancer [abstract]. In: Proceedings of the American Association for Cancer Research Annual Meeting 2018; 2018 Apr 14-18; Chicago, IL. Philadelphia (PA): AACR; Cancer Res 2018;78(13 Suppl):Abstract nr 3742.
- Pisano M, Hilas O. Zinc and Taste Disturbances in Older Adults: A Review of the Literature. Consult Pharm. 2016 May;31(5):267-70. doi: 10.4140/TCP.n.2016.267. PMID: 27178656.
- Maya Sultan, Orit Twito, Tali Tohami, Erez Ramati, Eran Neumark & Gloria Rashid Vitamin D diminishes the high platelet aggregation of type 2 diabetes mellitus patients. Pages 120-125 | Received 20 Jun 2017, Accepted 25 Sep 2017, Published online: 09 Jan 2018 https://doi.org/10.1080/09537104.2017.1386298
- Silvagno F, De Vivo E, Attanasio A, Gallo V, Mazzucco G, Pescarmona G. Mitochondrial localization of vitamin D receptor in human platelets and differentiated megakaryocytes. PLoS One. 2010 Jan 13;5(1):e8670. doi: 10.1371/journal.pone.0008670. PMID: 20107497; PMCID: PMC2809087
- Xia Luo, Qing Liao, Ying Shen, Huijun Li, Liming Cheng, Vitamin D Deficiency Is Inversely Associated with COVID-19 Incidence and Disease Severity in Chinese People, The Journal of Nutrition, Volume 151, Issue 1, January 2021, Pages 98–103, https://doi.org/10.1093/jn/nxaa332
- Isaia G, Giorgino R, Rini GB, Bevilacqua M, Maugeri D, Adami S. Prevalence of hypovitaminosis D in elderly women in Italy: clinical consequences and risk factors. Osteoporos Int. 2003;14: 577–582. doi:10.1007/s00198-003-1390-7
- Romagnoli, E., Caravella, P., Scarnecchia, L., Martinez, P., & Minisola, S. (1999). Hypovitaminosis D in an Italian population of healthy subjects and hospitalized patients. British Journal of Nutrition, 81(2), 133-137. doi:10.1017/S0007114599000264
- Sawako Hibino, Kazutaka Hayashida, Andrew C Ahn, Yasutaka Hayashida. Dynamic Change of COVID-19 Seroprevalence among Asymptomatic Population in Tokyo during the Second Wave. Medrxiv doi: https://doi.org/10.1101/2020.09.21.20198796
- Nakamura K. Vitamin D insufficiency in Japanese populations: from the viewpoint of the prevention of osteoporosis. Journal of Bone and Mineral Metabolism. 2005. pp. 1–6. doi:10.1007/s00774-005-0637-0
- Luxwolda MF, Kuipers RS, Kema IP, Dijck-Brouwer DA, Muskiet FA. Traditionally living populations in East Africa have a mean serum 25-hydroxyvitamin D concentration of 115 nmol/l. Br J Nutr. 2012 Nov 14;108(9):1557-61. doi: 10.1017/S0007114511007161. Epub 2012 Jan 23. PMID: 22264449
- William Douglass, MA. A Summary, Historical and Political, of the First Planting, Progressive Improvements and Present State of the British Settlements of North America, London, 1760 p 398.
- Dr Doyin Okupe in The News, 13 January 2021. https://www.thenewsnigeria.com.ng/2021/01/13/doyin-okupe-exposure-to-sunlight-is-why-covid-19-spares-the-poor/
- Dr David Grimes. Excess deaths from Black, Asian, and Minority Ethnic Doctors during the Covid-19 Pandemic http://www.drdavidgrimes.com/2020/11/Covid-19-vitamin-d-deaths-of-doctors.html
- John N Hathcock, Andrew Shao, Reinhold Vieth, Robert Heaney, Risk assessment for vitamin D, The American Journal of Clinical Nutrition, Volume 85, Issue 1, January 2007, Pages 6–18, https://doi.org/10.1093/ajcn/85.1.6
- Johanna M. Geleijnse, Cees Vermeer, Diederick E. Grobbee, Leon J. Schurgers, Marjo H. J. Knapen, Irene M. van der Meer, Albert Hofman, Jacqueline C. M. Witteman, Dietary Intake of Menaquinone Is Associated with a Reduced Risk of Coronary Heart Disease: The Rotterdam Study, The Journal of Nutrition, Volume 134, Issue 11, November 2004, Pages 3100–3105, https://doi.org/10.1093/jn/134.11.3100
- Veugelers PJ, Ekwaru JP. A statistical error in the estimation of the recommended dietary allowance for vitamin D. Nutrients. 2014;6(10):4472‐4475. Published 2014 Oct 20. doi:10.3390/nu6104472hyg
- Papadimitriou DT. The Big Vitamin D Mistake. J Prev Med Public Health. 2017 Jul;50(4):278-281. doi: 10.3961/jpmph.16.111. Epub 2017 May 10. PMID: 28768407; PMCID: PMC5541280.
- Dr John Campbell YouTube video 16 September 2020, Vitamin D and Pandemic science https://www.youtube.com/watch?v=ZqZLMoLvhgk
- Vitamin D supplementation guidance. Page 30-31. Nov 2020. https://issuu.com/cheltenhamlifestyleandbusiness/docs/cheltenham_20lifestyle_20_26_20business__20issue_2/30
- Laura A. G. Armas, Bruce W. Hollis, And Robert P. Heaney. Vitamin D 2 Is Much Less Effective than Vitamin D 3 in Humans. 2004 Jnl Clin End Metab. 89(11):5387-5391. Doi:10.1210/jc.2004-0360
- Jeroen H. F. de Baaij, Joost G. J. Hoenderop, and René J. M. Bindels. Magnesium in Man: Implications for Health and Disease. Physiological Reviews 2015 95:1, 1-4
- Carolyn Dean MD, ND. Book, The Magnesium Miracle. 15 August 2017. ISBN-10 : 0399594442 . ISBN-13 : 978-0399594441
- Noticias de la Junta11.20. Health will treat elderly in nursing homes with Calcifediol to mitigate the effects of Covid. Various studies demonstrate the protective capacity of vitamin D against acute respiratory infections: http://www.juntadeandalucia.es/presidencia/portavoz/salud/155979/ConsejeriaSaludFamilias/ConsejoGobierno/Covid/mayores/vitaminaD/calcifediol
- Andalucía Covid dashboard. http://www.juntadeandalucia.es/institutodeestadisticaycartografia/salud/COVID19.html
Last updated on 18th June 2021 by cytoffice



Why are there “winter pressures” on the NHS? Could this also be correlated with lower vitamin D levels? Were the pressures less when vitamin D levels were higher in the late 1900s?
Hi Shabra,
Yes, that is correct – winter pressures are absolutely correlated to vitamin D levels! This is the reason for winter pressures throughout the entire northern hemisphere and of course, if you look at Australia/New Zealand, you will find that their flu/respiratory illness season is reversed so that they have theirs in their winter which is during our summer months. There has long been discussion about the reason for this seasonality, with suggestions that humidity and/or temperature could play a part. However, I believe that the study referred to at the very end of section 5 which demonstrated that the only reasons for this seasonality can be vitamin D levels and/or UV light (of course UV is required to make vitamin D), also applies equally to all respiratory viruses. This phenomenon of seasonality and the vitamin D connection has been recognised for a very long time and certainly since R Edgar Hope-Simpson’s wrote his seminal book The transmission of Epidemic Influenza in 1992 but, unfortunately, it seems to have been forgotten even though the book had an excellent reception. It is not very well taught and seems to have been entirely lost to a generation of medics. [You can find a nice article on this topic in Virology here]
It is extremely difficult to make any meaningful comparison with the 1900’s as many factors influence the perceived pressure on hospitals. For instance, these will include differences in the proportion of elderly/susceptible people, differences in hospital bed/staff capacity, and any improvements in treatments.
Thanks,
Eshani
Fantastic article! I can’t profess to understanding it all as very technical. But in my view, if the right people read this it could be a game changer in the fight against Covid. Brilliantly written and evidenced
A most interesting and informative article. It saddens and annoys me intently when people in power, people who have the power,to put this information out there to the general public seem to keep it under wraps. I had been aware for some time that increasing your vitamin D levels can prevent Covid 19, and reading this report has certainly confirmed this.
Why is it whenever an holistic approach is ever mentioned as an alternative to conventional medicine it is poo pooed and put down. Surely to work with the body with vitamins, minerals etc is a much better treatment than blasting it with alien materials which can have in some cases very detrimental side effects.
Sadly again there appears to be a lot of money to be made within the big pharmaceutical companies and money seems to talk here! I don’t decry all convential medicine and yes it certainly does have its place, what I do decry is how holistic medicine always has to take a back seat over the two why is this? I can only put it down to money, there is obviously more money to be made within the large pharmaceutical companies than the smaller holistic ones, which is so unfair and makes me so angry.
Another interesting point made in your article re fats in our diet. Time and time again you hear especially woman say ‘ no can’t have that the fat content is too high’ and reach for an alternative which is usually full of artificial, low fat alternatives which have no use or benefit to the body whatsoever. Of course it does however have the ‘low fat’ slogan plastered all over the packaging so bingo people fall for this immediately!!!
It is, and I feel increasingly difficult for science and holistic thinking to be made aware to the general public, after all to work in harmony with your body seems to be logical to me but sadly I feel I am in the minority.
Hi Judy,
I couldn’t agree more with your observations and statements! As Dr Aseem Malhotra, the outspoken consultant cardiologist, who has bravely tried to correct misinformation about fats, recently tweeted, Big Food and Bad Pharma have a lot to answer for! I am a glad you mention fats as this such a hugely important issue. It is a testimony to the manipulative power of marketing that so many of us have replaced nutrient dense natural fats containing many valuable fat-soluble vitamins and other essential nutrients necessary for the human body and brain, and which humans have eaten for millennia, with processed carbohydrates, artificial ingredients, and nutrient poor foods. Precisely the types of foods that makes people hungrier and therefore fatter. Luckily, there are many amazing highly qualified and passionate ambassadors for fats besides Dr Malhotra and I would encourage anyone to watch very informative you tube videos on the subject of fats, cholesterol and seed oils featuring Dr Malhotra or any of the following: Dr Nina Teicholz, cardiologist Dr Nadir Ali, Ivor Cummings (The Fat Emperor) and Dr Zoe Harcombe.
Thanks,
Eshani
This is an excellent, evidence-based article – thank you! (It would be great if it could be circulated more widely somehow.)
Excellent information and analysis. Many thanks. Keep up the good work. A pity more doctors and politicians are not more aware of the importance of vitamin D, especially at higher doses, and to educate the public .
One of the best articles you have ever posted, IMO. I have been a strong advocate for vitamin D supplementation for years. I have even been a guest on various podcasts & have promoted your products to literally thousands of people. I am a social influencer in the world of stocks & I even have a health & wellbeing room in my online academy for my students. Many of which now supplement D3 & K2.
Thank you for your continued work in this vital field & thank you for sharing life-saving information.
Excellent review of studies including shortfalls of the medical community’s acceptance and understanding. This entire past year has revealed the blatant prejudice of the medical community in looking for answers to save people’s lives from anything other than drugs or vaccines. The very cure for a variety of forms of cancer may already exist in natural form somewhere, but the medical community will never find it. They are not looking to actually prevent and heal people of illnesses, they are only looking for ways to develop and use drugs.
One side note to address a pet peeve, I really do wish operational science articles would leave out references to evolutionary philosophy for claims. It has no place as it is conjecture at best, cannot be proven. This article’s oxymoronic statement that “evolution designed” is quite laughable. The very philosophical argument behind evolution is that life allegedly arose from random accidents with no guidance other than trial and error. That is not design. Design requires a legitimate developer, one might call it a creator, that deliberately engineers something in a specific way with specific processes to operate. Evolution is not an entity that can create anything by purposeful, intentional design. But, we were actually designed by an intelligent source, God. So please, just leave out the unfounded philosophical conjecture which reveals contradictory thinking from future blog articles.
Hi!
Thank you very much for this detailed information. It is extremely useful and made a lot of sense. I have one question though that I would really appreciate clarification on. You are saying that in order to maintain sufficient levels of Vitamin D in the system one would need 6000-10000IU. On my packet of Cytoplan Vitamin D though the recommendation is t take 1 tablet per day which equals 1000IU if I understand the packet description correctly. It also says ‘do not exceed the recommended daily intake’. i find this a contradiction, as the 1000IU recommended on the packet is a fraction of what this article says one needs as a daily intake. Could you clarify this please?
Many thanks,
Sabine
Hi Sabine,
The product we have which is 1,000i.u. is for juniors – in the main children from 8-10 years old. The wording “do not exceed the recommended dose” is a legal requirement for all supplements. This dose for juniors is in keeping with Government recommendations, this is not an adult product. Our experience of the amount needed to maintain optimum Vit D blood levels is that most people need to take between 3,000 i.u and 5,000 i.u/day although there is evidence emerging that some people need more and it is indeed safe to take more. This is a rapidly changing landscape as new research better understands the physiological role of Vitamin 3. The NHS say that an optimum level is over 80nmols/L. Our view would be that 100-150nmols/L is more optimal at this time where a good vitamin D status has been shown to be protective against Covid by virtue of it role in T cell immunity and other protective mechanisms. The NHS also say that a level of over 220nmols/L is too high. The only way individuals can know how much they need to take to maintain optimum status is by taking a set level consistently for a while alongside testing blood levels every few months. 10 years ago Vitamin D was thought to be unsafe in levels above the RDA as it was then of 5ug – but that has changed in recent years and it is now known to be very safe indeed at high levels with little if any risk of toxicity. As I mentioned earlier this whole area of nutrition and science is a rapidly changing landscape.
Thanks,
Amanda
Thank you for publishing this research – I have spent the past year telling friends and family to supplement with Vit D to safeguard them from Covid 19. (I know this as Kinesiology indicates this is the primary need from the body of anyone who has presented with Covid-19). Please get this information out to the world via Government/Media as so many lives could be saved with this knowledge. Everyone needs to know this.
Hi Sue,
Thank you for your positive comments. The information is also available for public access via the Open Science Framework server and has been shared on social media. It would be great if you could share the link to the Cytoplan blog as widely as possible. Unfortunately, as far as the government goes, although David Davis MP has been championing the cause as much as he possibly can, it seems that the Health Secretary and his advisors’ have little time for it. Under pressure from David Davis, they did finally start giving out vitamin D to care homes but the doses of 400 IU are far too low to make much difference and were given far too late in the season. We all now need to do our own research in order to remain healthy – it is clear that we cannot rely on the Government to have our best interest at heart when they continually have powerful and wealthy pharmaceutical and food industry lobby groups at their door.
Thanks,
Eshani
I live in England but spend my winters in Austria. I take vit D suppliments over the winter but not the summer. When outside ( i cycle and golf a lot) i use sun tan cream but if this depletes the amount of vit D i absorb from the sun what is the alternative to protect myself from UV rays ?
Hi Jan,
Here is some information that might put your mind at rest, taken from section 8 of my previous blog on this topic (here): “Concerns about cancer dangers from sun exposure may be misconstrued. Almost 90% of skin cancer deaths are caused by melanoma. Although there is an association between excessive sun exposure and non-melanoma skin cancers, and excessive sun exposure or burning should be avoided, there is no credible scientific evidence that moderate sun exposure can cause melanoma [17,77,61,62]. Working indoors and lack of vitamin D is associated with a significantly increased risk of melanoma while occupational sun exposure is associated with reduced risk of melanoma [77]. Melanoma is more often found in areas which are not exposed to the sun [17,62]. There are other risk factors for melanoma such as being obese, high alcohol consumption and being sunburnt when young, but sun exposure in the present which is no more than moderate is not a risk factor. Ironically, 83% of Australian dermatologists were found to be vitamin D deficient [29].
The dangers and extensive ill effects on health of a lack of moderate sun exposure and consequential lack of vitamin D, appears to, by far, outweigh any health benefit from avoiding it. It is possible that sun exposure may have other unknown positive effects on the human body besides making vitamin D. A Swedish 20 year follow up study of almost 30,000 women found that avoidance of sun exposure is a risk factor for death of similar magnitude as smoking! [89].”
Professor Holick, the world renown US based vitamin D researcher who has probably been researching vitamin D for longer than anyone else on the planet advises that people should initially expose their skin for a short period each day without any sun-tan cream. The period advised is different for everyone depending on the exposure time needed for the skin to turn pale pink the following day. Burning should, of course, be avoided. Professor Holick’s exposure guidelines can be found here on Dr Ruscio’s page: https://drruscio.com/sun-exposure-and-vitamin-d-levels-with-dr-michael-holick/ Professor Holick has also produced a helpful app which you can download called the Dminder App. Details can be found here. This short commentary by Dr Kendrick is also helpful.
I hope these are helpful.
Thanks,
Eshani
cWell done, why are the media not interested
Hi Carole,
The media have shown interest and have published many stories on the benefit if Vit D during the Covid pandemic. Unfortunately, it appears that despite the mounting evidence the Government have yet to be convinced and this view is having an influence on what the press say. Plus, I feel the press would not want people to feel that if they take Vitamin D they are safe and do not have to worry about the risk of Covid 19.
Thanks,
Amanda
This makes incredible reading. It is just so sad that the ‘powers that be’ so to speak are not acting on something so simple & easily administered.
We as a family have always taken Vit D albeit only during the winter months, but certainly after having read this article that will be changing.
Thank you for sharing such an informative article.
Thank you for dispatching the best known facts on vitamin D. It was beautiful to read as I have watched the individual trials come out and be ignored over a year when many thousands of lives might have been saved. Please keep holding their feet to the fire.
Spent a bit of time on this topic, and wondered why it is that we use UVB as an energy source to start the production of vitamin D. Then I realised that other animals with fur on – such as cattle, horses etc – do the same thing. UVB can penetrate their hair, which is probably why it is used at all. This is also why white-fur animals (to our eyesight) look grey to the predators with UV sensitive eyes (e.g. wild wolves) when hunting on a snowfield. We would have had a lot more hair on as well, many years ago. Of course, we’ve manufactured our own way of preventing it getting through at all; shame.