In this week’s article we provide a roundup of some of the most recent health and nutrition related articles to make the news, six items comprising:
- Diabetes: Children ‘not getting recommended checks’
- High dose vitamin D may boost diversity of the gut microbiome: Study
- UK doctors told to halve inappropriate antibiotic prescriptions by 2020
- Official advice on low-fat diet and cholesterol is wrong, says health charity
- Connections between gut microbiota and the brain
- Early introduction of allergenic foods reduces risk of food sensitization, study suggests
Diabetes: Children ‘not getting recommended checks’
“Almost 75% of older children in England and Wales with diabetes are not getting key health checks, a study suggests.
Data from 27,682 children and young people showed 25.4% of those aged 12 and older had all seven recommended annual checks, such as eye screenings.
However, the Royal College of Paediatrics and Child Health, which carried out the audit, says the overall picture is one of improving care.
Diabetes UK said missed health checks for children was “very worrying”.
Health officials recommend all children with diabetes should be assessed to ensure they are managing their condition properly.
Guidelines from NICE (National Institute for Health and Care Excellence) state that all children with diabetes should have their blood sugar levels checked every year and those over the age of 12 should also have six other annual health checks.
These include measures of growth, blood pressure, kidney function, cholesterol, as well as an eye screening and a foot examination.”
Related Cytoplan blogs
Could Alzheimer’s disease be ‘Type 3 Diabetes’?
Diabetes and Insulin Resistance
Cognitive and Emotional Approaches to Reversing Insulin Resistance
Dietary Approaches to Reversing Insulin Resistance
High dose vitamin D may boost diversity of the gut microbiome: Study
“Vitamin D3 may increase bacterial richness in the upper gastrointestinal tract and reduce opportunistic pathogens, says a new study from Austria.
Scientists from the Medical University of Graz report that high daily doses of vitamin D3 for five weeks led to significant reductions in bacteria such as Pseudomonas SPP and Escherichia/Shigella SPP.
“The marked reduction in Gammaproteobacteria, which include typical opportunistic pathogens and the increase in phylotype richness, supports the beneficial effect of a high-dose vitamin D3 supplementation on the human gut microbiome”, wrote the researchers.
“This might in part explain the effects of a vitamin D-rich diet on IBD or bacterial infections and encourage studying the effects of vitamin D in these patients.”
The researchers recruited 16 healthy people to participate in their open-label, pilot study. Participants had their GI tracts sampled at four different places, starting with the stomach and ending with a stool sample, before and after receiving high dose vitamin D3 for eight weeks.
The dose for the first four weeks was 980 IU/kg bodyweight of vitamin D3 per week, and the dose for the second four weeks was 490 IU/kg bodyweight per week.”
Related Cytoplan blogs
“Greeting from both myself and my Microbiome” – Dr Rangan Chatterjee
Dr Rangan Chatterjee – A talk on ‘Good Gut Health’
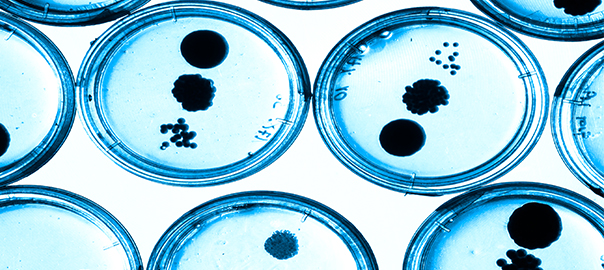
UK doctors told to halve inappropriate antibiotic prescriptions by 2020
“Tough new targets to curb the overuse of antibiotics and cut the risk of the resurgence of killer diseases have been announced by the government, which will require doctors to halve the number of inappropriate prescriptions written for the drugs by 2020.
David Cameron told world leaders at the G7 summit in Japan that the issue was a priority for him, as he revealed plans to crack down on prescribing within the UK. Experts warn that unless action is taken drug-resistant infections will kill more people than cancer, taking 10 million lives a year by 2050.
Inappropriate prescribing of antibiotics – for instance for infections such as coughs and colds caused by a virus rather than bacteria – is to be halved within the next four years.
Officials say 10% of the 34m antibiotics prescribed each year are handed to people inappropriately, suggesting a target reduction of 1.7m prescriptions annually by 2020.”
Related Cytoplan blogs
Antibiotic Resistance – ‘The Ticking Time Bomb’
Antibiotics, Diarrhoea & Probiotics
Official advice on low-fat diet and cholesterol is wrong, says health charity
“Urging people to follow low-fat diets and to lower their cholesterol is having “disastrous health consequences”, a health charity has warned.
In a damning report that accuses major public health bodies of colluding with the food industry, the National Obesity Forum and the Public Health Collaboration call for a “major overhaul” of current dietary guidelines. They say the focus on low-fat diets is failing to address Britain’s obesity crisis, while snacking between meals is making people fat.
Instead, they call for a return to “whole foods” such as meat, fish and dairy, as well as high-fat, healthy foods including avocados, arguing: “Eating fat does not make you fat.”
The report – which has caused a huge backlash among the scientific community – also argues that saturated fat does not cause heart disease while full-fat dairy, including milk, yoghurt and cheese, can actually protect the heart.
Processed foods labelled “low fat”, “lite”, “low cholesterol” or “proven to lower cholesterol” should be avoided at all costs, and people with type 2 diabetes should eat a fat-rich diet rather than one based on carbohydrates.”
Related Cytoplan blogs
Why a Low Fat Diet and Statin’s May Cause Alzheimer’s
Connections between gut microbiota and the brain
“The gut microbiome is the aggregate of human gut microorganisms with all its bacteria, archaea, viruses and fungi.
For a long time, it seemed far-fetched to think that the microbiome could also be responsible for processes outside the digestive tract. Yet the scientific community keeps uncovering further amazing details. Recent studies on laboratory animals which grow up without any microorganisms (germ-free) show for example that microorganisms in the gut are even capable of influencing behaviour.
Dr Lepage: “Intestinal microbes can verifiably produce neuromediators that have an effect on the brain. Germ free mice showed less anxiety than their conspecifics whose gut was populated with commensal microbiota. However, there is only scant evidence thus far on how this process works in the human brain.”
It has been proven in the meantime that the gut and the brain communicate with each other via several routes including the vagus nerve, the immune system, the enteric nervous system or by way of microbial metabolic processes.
For instance, intestinal bacteria convert carbohydrates into short chain fatty acids, e.g. in butyric acid. This strengthens the connections between the cells and reinforces the blood-brain barrier, which serves as a cellular wall to protect the brain from infections and inflammations.”
Early introduction of allergenic foods reduces risk of food sensitization, study suggests
“Children who had a diet that included cow’s milk products, egg and peanut before age one were less likely to develop sensitization to the corresponding foods, according to new research presented at the ATS 2016 International Conference. Early introduction of eggs appeared to be especially beneficial, as it decreased the risk of sensitization to any of the three tested foods.
The Canadian Healthy Infant Longitudinal Development (CHILD) Study, directed by Malcolm Sears, MB, ChB, professor in the Department of Medicine at McMaster University, is believed to be “the first to determine the effects of timing of food introduction to cow’s milk products, egg, and peanut, on food sensitization at age one in a general population-based cohort,” said lead investigator Maxwell Tran, a research student at McMaster University in Hamilton, Ontario, Canada.
Most previous studies focused on one specific food type, studied outcomes in later childhood or studied high-risk groups.
The study included data from 1,421 children. Most parents in the study introduced cow’s milk products, which encompass cow’s milk-based formula, to their infants before age one: 0-6 months 48 percent, 7-12 months 48 percent and 2 months 4 percent. The majority of parents, however, delayed introducing eggs to their children: 0-6 months 6 percent, 7-12 months 76 percent and 12 months 19 percent.
“The clinical implications of our findings are that early introduction of allergenic foods (egg, cow’s milk products, and peanut) before age one should be encouraged and is better than food avoidance for reducing the risk of food sensitization,” said Mr. Tran. “Sensitization is not the same as allergy, but it is an important step on the pathway.””
Related Cytoplan blogs
Hay Fever, Allergies and the Allergic Reaction
Elimination Diets – Pinpointing the Source of Undiagnosed Symptoms
If you have any questions regarding the topics that have been raised, or any other health matters please do contact me (Amanda) by phone or email at any time.
amanda@cytoplan.co.uk, 01684 310099
Amanda Williams and the Cytoplan Editorial Team: Joseph Forsyth, Simon Holdcroft and Clare Daley
Last updated on 1st June 2016 by cytoffice

We’d love your comments on this article
It’s easy, just post your questions, comments or feedback below