Pain afflicts millions of people worldwide and continues to be prevalent due to its complex pathogenesis. The body is a complex system that can be negatively affected by many factors in life, such as poor diet, lack of exercise, injury and illness, and environmental factors such as stress or toxin exposure.
These contributing factors can lead to a substantial impact on the body and can cause inflammation and pain. Diet and lifestyle modifications can therefore play an important role in the management of pain as they can help address underlying causes, such as inflammation, help manage symptoms and restore function.
In this week’s blog we will take a look at some of nature’s pain relievers and other ways of naturally managing pain.
Pain Management Statistics
Opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), antidepressants, and other pharmacological agents remain a central component of pain management.1 For instance, an estimated 7.1 million adults in England use prescription opioids for pain2, and while these are perhaps necessary in certain circumstances, for those who suffer with long-term, chronic or regular pain, they can be habit-forming, often cause side effects, deplete nutrients, and may cause lasting damage.
The NHS states that there is little evidence that these painkillers are helpful for long-term pain.3 Their usage, however, has more than doubled from 1998 to 2018 and has now been referred to as the opioid epidemic in the UK.2
In addition, around 200 million packs of paracetamol are sold without prescription in the UK every year, which equates to an average of 70 paracetamol tablets per person.4 NSAIDs are also one of the most commonly prescribed pain medications which are effective for pain and inflammation although they are known for multiple adverse effects.5
In 2016, research showed that between a staggering third and half of the UK population (around 28 million adults) are living with persistent pain.6 This figure is likely to be even higher now, with the incidence of chronic pain being greater than that of heart disease, diabetes, and cancer combined.7
Given the ongoing challenges of pain management, exploring other effective and safer alternatives are needed.
Inflammation and its role in pain
Inflammation is part of the body’s immediate response to injury or infection, but uncontrolled inflammation damages tissues and plays an important role in the pathology of many diseases of which pain is a symptom.
Natural pain management – effective herbs, vitamins, minerals and other compounds
Our natural world is abundant in plants that can exert analgesic and anti-inflammatory action on the body, and many have had a long history of use.
Boswellia
Boswellia is an Ayurvedic herb with anti-inflammatory properties and has been investigated for its benefits in conditions such as osteoarthritis (OA). Osteoarthritis is the most common joint disease worldwide, affecting an estimated 10% of men and 18% of women over 60 years of age.1
It has been shown that oral Boswellia supplements can significantly suppress the pain and immobility associated with OA, with the effects being felt in as little as one week.2 In support of this, a recent systematic review and meta-analysis showed that Boswellia can be an effective and safe treatment option for patients with OA.3
Boswellia has been shown to inhibit the 5-lipoxygenase pathway, thus playing a positive role in various inflammatory diseases that are perpetuated by the production of leukotrienes. Pharmaceutical drugs that work to prevent this enzyme are used in the treatment of inflammatory conditions including arthritis, and ulcerative colitis.4
As well as reducing inflammation, it is thought that Boswellia’s mechanism of action on joints also includes the prevention of GAG degradation and improved blood supply to joint tissues.
Curcumin
Turmeric’s main active component is curcumin, which is what gives the spice its bright colouring. Curcumin is well-known for its anti-inflammatory properties and can aid in the management of oxidative and inflammatory conditions. It has been shown to help in the management of exercise-induced inflammation and muscle soreness, thus enhancing recovery and performance in active people.1
In a recent meta-analysis, curcumin was shown to improve symptoms and inflammation levels in people with arthritis and in a systematic review this year, curcumin was shown to be equally as effective as conventional therapies in alleviating pain in the orofacial region.2
One of its mechanisms of action is inhibiting Cox-2 enzymes which produce inflammatory prostaglandins. The major therapeutic actions of NSAIDs are primarily enacted by their ability to block certain prostaglandin synthesis through the cyclooxygenase enzymes (COX-1 and COX-2) inhibition.3 Curcumin is recognized as a safe and well-tolerated compound.
CBD
We all have an endocannabinoid system, which is comprised of endogenous cannabinoids and cannabinoid receptors. CBD works by acting on the cannabinoid receptors in the human body. These receptors exist because the human body produces its own cannabinoids, which can influence several bodily processes including pain.
One of the most notable benefits of CBD oil is its ability to relieve pain naturally and research on CBD products and pain management continues to emerge with effective results.
Omega 3
Reducing foods high in omega 6 (farmed meats, dairy products and vegetable oils) can be of benefit when tackling pain and inflammation as they can be inflammatory. This is because they are high in the omega 6 fat arachidonic acid or linoleic acid (precursor to arachidonic acid), which can be converted to the pro-inflammatory prostaglandin PGE.
Increasing sources of omega 3 from oily fish and/or a supplement containing EPA is recommended as EPA is converted into anti-inflammatory prostaglandins in the body. The ability of omega-3 fatty acids to interfere with arachidonic acid metabolism is at the heart of their proposed anti-inflammatory effects.1
In a systematic review and meta-analysis carried out this year, it was shown that supplementing with omega-3 may improve inflammatory rheumatic disease activity and might be an adjuvant therapy in rheumatoid arthritis.2 Another study demonstrated its ability to alleviate pain in rheumatoid arthritis patients.3
In further research, omega-3 has been shown to moderately improve chronic pain, especially in relation to dysmenorrhea (throbbing or cramping pains in the lower abdomen during menstruation).4 Furthermore, in a study that compared ibuprofen and omega-3, the results demonstrated an equivalent effect in reducing arthritic pain.5
Magnesium
Magnesium exerts its analgesic effects by blocking the N-methyl-d-aspartate (NMDA) receptors (which are active contributors to pain transmission)1 and thus, the prevention of central sensitisation.
Many studies have found that magnesium has beneficial effects in those suffering from neuropathic pain, dysmenorrhea, tension headache, muscle cramps, acute migraine attack, and more.2
Magnesium formulations when coupled with amino acids, such as L-threonate or glycinate, may work better for migraine. In fact, magnesium threonate is the only magnesium shown in studies to cross the blood-brain barrier.
Collagen
Collagen is the most abundant protein in the human body. While there are several types of collagen proteins, it is collagen type II protein which makes up the fluids and supports function in the cartilage and joints.
Cartilage is the main connective tissue in the body, and it protects the ends of bones in joints by providing padding, lubrication and tensile strength. Hence, it keeps joints sliding, bending and moving smoothly.
Cartilage damage is a frequent cause of joint pain and can be from injury, or wear and tear. In addition, the body’s ability to produce collagen naturally declines with age. As such, supplementary collagen has been suggested as a possible way to mitigate the effects of this decline. Type I collagen has also been shown to help improve muscle strength and support bone health.
The results of a recent meta-analysis showed that collagen was effective in improving OA symptoms, which included reduced pain, stiffness and improved mobility.1 In further studies, collagen administration resulted in a 32% decrease in joint pain and a 44% improvement in stiffness among women with osteoarthritis.2 In a 24-week clinical trial, improved joint health and a reduced risk of joint deterioration in athletes was observed following supplementation with hydrolysed collagen.3
MSM
MSM is an organic form of sulphur, and an important building block for healthy bones and joints. It is found in collagen and elastin, which are proteins found in the connective tissue in skin, joints, muscles, bone and blood vessels.
In a study of individuals over the age of 50, it was found that treatment with a supplement containing MSM for 12 weeks decreased pain, stiffness and swelling in the joints, compared to a placebo.1
MSM may also reduce exercise-induced muscle damage and pain and increase antioxidant activity.2 MSM can reduce the release of molecules associated with inflammation and pain, such as TNF-ɑ and IL-6.
Taurine
The fundamental role of taurine in the immune system is related to its antioxidant properties. Taurine protects tissues from oxidative stress associated with the pathology of various inflammatory diseases. It has been shown to reduce inflammatory cytokines which contribute to the inflammatory response in conditions such as rheumatoid arthritis. It also helps to prevent muscle damage and soreness. Certain diets, particularly vegetarian or vegan diets, may lack adequate amounts of taurine.
The impact of diet on pain management
The food choices that we make can either make our body more inflamed or less inflamed, and hence more or less at risk of pain. An anti-inflammatory diet which is rich in fruit and vegetables, lean protein, healthy fats and herbs and spices, with minimal amounts of red meat, sugar, and processed foods is therefore recommended to help address inflammation in the body.
Lifestyle and exercise as a key tool in natural pain management
Beyond nutrition, lifestyle can play a significant role in pain management, particularly exercise. While exercising may be the last thing you feel like doing when you’re in pain, it can also be key to managing pain too. For example, gentle exercise has been shown to:1
- build muscle strength and flexibility
- reduce stiffness
- reduce pain and sensitivity
- improve sleep
- reduce fatigue
- reduce inflammation
- improve mood
- increase immune function
- reduce stress levels
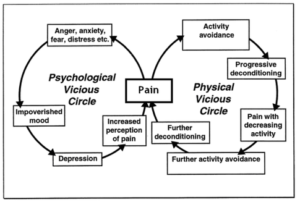
All of these factors have been implicated in pain and the development of pain. An example of the self-limiting cycle of pain can be illustrated below:2
Stress Management Techniques
Stress can make pain worse. It can cause muscles to tense or spasm, increasing pain. When we experience prolonged stress, levels of the hormone cortisol rise, which overtime can cause inflammation and pain.
Relaxation can be very helpful in reducing stress and relieving muscle tension, aches and pains. It can also promote sleep, needed for the repair and regeneration of the body.
Breathing exercises, massage, meditation and yoga are all good ways to relax and reduce stress. Ashwagandha is an adaptogenic herb, which may support a sense of calm and relaxation. Other nutrients to consider include magnesium, the B vitamins, vitamin C and l-theanine.
Sleep
Sleep and pain appear to have a bidirectional relationship and researchers have found that inadequate sleep and poor sleep quality often causes heightened sensitivity to pain.1 Poor sleep can also affect our ability to move and exercise, our mood, and can increase inflammation in the body.
Nutrients such as magnesium, vitamin B6, glycine, L-theanine, and natural sources of melatonin such as acerola cherry can support restful sleep.
Mind-set
Research suggests that pain involves both the mind and the body and has both a biological and psychological component. Mind-body therapies (healing techniques that enhance the mind’s interactions with bodily function) may therefore have the capacity to alleviate pain by changing the way we perceive it.
Brain-imaging research has shown a negative pain mind-set (ruminating on how awful pain is and expecting it to worsen) actually amplifies pain processing in the brain.1 .
Key Takeaways
- Diet and lifestyle modifications can help in the management of pain as they help address underlying causes, help manage symptoms and restore function
- Opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and antidepressants remain a central component of pain management but are known for multiple adverse effects
- It has been shown that oral Boswellia supplements can significantly suppress the pain and immobility associated with OA
- Curcumin is well-known for its anti-inflammatory properties and can aid in the management of oxidative and inflammatory conditions
- Most notable benefits of CBD oil is its ability to relieve pain naturally. Research continues to emerge with effective results
- Supplementing with omega-3 may improve inflammatory rheumatic disease activity and might be an adjuvant therapy in rheumatoid arthritis
- Many studies have found magnesium has beneficial effects for neuropathic pain, dysmenorrhea, tension headache, muscle cramps, acute migraine attack
- Collagen is needed for cartilage to protect the ends of bones in joints by providing padding, lubrication and tensile strength
- MSM is an important building block for healthy bones and joints
- The food choices that we make can either make our body more inflamed or less inflamed. Following an anti-inflammatory diet is recommended
- Exercise can also be key to managing pain
- Relaxation can be very helpful in reducing stress and relieving muscle tension, aches and pains
- Sleep and pain have a bidirectional relationship
Natural Pain Management Refs
Statistics
- Park, R. et al. (2020) ‘Efficacy and safety of magnesium for the management of chronic pain in adults: A systematic review’, Anesthesia and Analgesia, 131(3), pp. 764–775.
- Public Health England, (2019)
- NHS England — South West » Opioid prescribing for chronic pain. Available at: https://www.england.nhs.uk/south/info-professional/safe-use-of-controlled-drugs/opioids/ (Accessed: 18 October 2022).
- Sheen, C.L. et al. (2002) ‘Paracetamol pack size restriction: The impact on paracetamol poisoning and the over-the-counter supply of paracetamol, aspirin and ibuprofen’, Pharmacoepidemiology and Drug Safety, 11(4), pp. 329–331.
- Wongrakpanich, S. et al. (2018) ‘A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in The Elderly’, Aging and Disease, 9(1), p. 143.
- Fayaz, A. et al. (2016) ‘Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies’, BMJ Open, 6(6), p. e010364.
- Incorporating Functional Medicine Into Chronic Pain Care (2020). Available at: https://www.practicalpainmanagement.com/treatments/incorporating-functional-medicine-chronic-pain-care (Accessed: 17 October 2022).
Boswellia
- Prevalence | Background information | Osteoarthritis | CKS | NICE (2022). Available at: https://cks.nice.org.uk/topics/osteoarthritis/background-information/prevalence/ (Accessed: 21 October 2022).
- Pizzorno JE, Murray MT. Textbook of Natural Medicine 4th Ed. 2013. Elsevier
- Yu, G. et al. (2020) ‘Effectiveness of Boswellia and Boswellia extract for osteoarthritis patients: a systematic review and meta-analysis’, BMC complementary medicine and therapies, 20(1).
- Fischer, A.K. and Mullin, G.E. (2012) ‘Inflammation and nutraceutical modulation’, Bioactive Food as Dietary Interventions for Arthritis and Related Inflammatory Diseases: Bioactive Food in Chronic Disease States, pp. 337–345.
Curcumin
- Hewlings, S.J. and Kalman, D.S. (2017) ‘Curcumin: A Review of Its’ Effects on Human Health’, Foods, 6(10).
- Sterniczuk, B. et al. (2022) ‘Effectiveness of Curcumin in Reducing Self-Rated Pain-Levels in the Orofacial Region: A Systematic Review of Randomized-Controlled Trials’, International journal of environmental research and public health, 19(11).
- Wongrakpanich, S. et al. (2018) ‘A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in The Elderly’, Aging and Disease, 9(1), p. 143.
Omega 3
- Surette, M.E. (2008) ‘Mechanisms and innovations: The science behind dietary omega-3 fatty acids’, CMAJ : Canadian Medical Association Journal, 178(2), p. 177.
- Sigaux, J. et al. (2022) ‘Impact of type and dose of oral polyunsaturated fatty acid supplementation on disease activity in inflammatory rheumatic diseases: a systematic literature review and meta-analysis’, Arthritis research & therapy, 24(1).
- Senftleber, N.K. et al. (2017) ‘Marine Oil Supplements for Arthritis Pain: A Systematic Review and Meta-Analysis of Randomized Trials’, Nutrients, 9(1).
- Prego-Domínguez, J., Hadrya, F. and Takkouche, B. (2016) ‘Polyunsaturated Fatty Acids and Chronic Pain: A Systematic Review and Meta-analysis’, Pain physician, 19(8), pp. 521–535.
- Maroon, J.C. and Bost, J.W. (2006) ‘Omega-3 fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain.’, undefined, 65(4), pp. 326–331.
Magnesium
- Park, R. et al. (2020) ‘Efficacy and safety of magnesium for the management of chronic pain in adults: A systematic review’, Anesthesia and Analgesia, 131(3), pp. 764–775.
- Na, H.S., Ryu, J.H. and Do, S.H. (2011) ‘The role of magnesium in pain’, Magnesium in the Central Nervous System, pp. 157–166.
Collagen
- García-Coronado, J.M. et al. (2019) ‘Effect of collagen supplementation on osteoarthritis symptoms: a meta-analysis of randomized placebo-controlled trials’, International Orthopaedics, 43(3), pp. 531–538.
- iang I-X et al (2014) ‘Collagen Peptides Improve Knee Osteoarthritis in Elderly Women A 6-Month Randomized, Double-Blind, Placebo-Controlled Study’ Agro Food Industry High Tech, 25 (2), pp. 19-23.
- Clark KL et al (2008) ’24-Week study on the use of collagen hydrolysate as a dietary supplement in athletes with activity-related joint pain.’ Curr Med Res Opin, 24(5), pp. 1485-1496.
MSM
- Xu, G. et al. (2015) ‘Evaluation of the Effect of Mega MSM on Improving Joint Function in Populations Experiencing Joint Degeneration’, International Journal of Biomedical Science : IJBS, 11(2), p. 54.
- Withee, E.D. et al. (2017) ‘Effects of Methylsulfonylmethane (MSM) on exercise-induced oxidative stress, muscle damage, and pain following a half-marathon: A double-blind, randomized, placebo-controlled trial’, Journal of the International Society of Sports Nutrition, 14(1).
Exercise
- Ambrose, K.R. and Golightly, Y.M. (2015) ‘Physical exercise as non-pharmacological treatment of chronic pain: Why and when’, Best Practice and Research: Clinical Rheumatology, 29(1), pp. 120–130.
- Emotions & the Pain Cycle – Oasis Massage. Available at: https://www.oasismassage.biz/blog/emotions-the-pain-cycle (Accessed: 21 October 2022).
Sleep
- Tang, N.K.Y. et al. (2012) ‘Deciphering the temporal link between pain and sleep in a heterogeneous chronic pain patient sample: a multilevel daily process study’, Sleep, 35(5), pp. 675–687.
Mind-Set
- Shpaner, M. et al. (2014) ‘Unlearning chronic pain: A randomized controlled trial to investigate changes in intrinsic brain connectivity following Cognitive Behavioral Therapy’, Clinical, 5, pp. 365–376.
If you have questions regarding the topics that have been raised, or any other health matters, please do contact our team of Nutritional Therapists.
nutrition@cytoplan.co.uk
01684 310099
Last updated on 3rd January 2024 by cytoffice



Another informative article. I learn so much from them. Thank you. I’m also a fan of Cytoplan supplements and take them daily as I have an autoimmune disease which benefits from healing from the inside out.
Hello there! Thanks so much for your kind comment – thrilled you find the blogs so useful!
To whom it may concern,
Another brilliant blog! I don’t always tell you, but I always enjoy reading them!
Best Wishes
Nicole Hopkins
Hi Nicole, thank you so much for your kind comment! We are so pleased to hear this!
What is Cytoplans answer to the article?
As everyone is individual, they may require different nutrients to address the pain they are experiencing. If you would like to receive a tailored supplement protocol, please email our team of nutritional therapists on nutrition@cytoplan.co.uk
Excellently comprehensive.
Thank you
This a very insightful blog on Pain and Management. I have nerve pain from Carpal Tunnel and I do much of what is recommended in this article.
In relation to Vitamins, how does one know what would be helpful to take to assist a there are several? I am looking for a registered Naturopath as I believe they can arrange blood tests?
If you are specifically referring to vitamins, I would recommend a comprehensive multivitamin and mineral formula to help cover any potential nutritional shortfalls. There is evidence of the B vitamins, and more specifically B6 and B12 being particularly supportive for those with Carpal Tunnel. In terms of the nutrients mentioned in this blog, as Carpal Tunnel is an inflammatory condition, supplements such as Boswellia or Curcumin, as well as ensuring an adequate intake of Omega 3 fatty acids, would be advised.
I love your informative blogs – thank you!
I only wish I could still receive your supplements here in Spain – Since ‘Brexit’ Customs have made it impossible to afford my orders.
I have real trouble sourcing good quality supplements over here. I am not back in the UK for at least 7 months so will have to order from you before I visit to get my much needed supplies delivered to a relative for me to collect.
Hi Lorni, thanks for your comments. We are sorry to hear you’ve experienced some difficulties. We escalated your comments to our Customer Services Manager and she replied advising that she was not aware of any issues in Spain – if you are happy to contact the customers services team on info@cytoplan.co.uk, we can investigate what happened when you last ordered from us.
An excellent, very informative article and well researched. Thanks Mo
Thank you!
A relative has been diagnosed with ME/CFS as well as coeliac.
How can she be helped holistically ?
Hi Jan, thanks for your comments. Magnesium supports energy production and may have a beneficial effect on pain. The B vitamins are also great for energy and adrenal support. There are a number of natural pain relievers mentioned in the blog too as well as a range of lifestyle suggestions. Due to the diagnosis of coeliac disease, paying close attention to any underlying gut issues/damage is also going to be key to overall health.
However, as everyone is individual, they may require different nutrients to address the pain or other symptoms they are experiencing. It may be worthwhile therefore asking your relative to fill out a health questionnaire which is available online on our website under the tab “nutrition advice” so we can gain a better picture of the symptoms they are experiencing. Alternatively, they can email our team of nutritional therapists on nutrition@cytoplan.co.uk
Very informative and key points are so helpful when time is short.
Thank you, Ann. So glad you find them helpful.