Vitamin B12 is a class of chemically related compounds, also called cobalamins that contain cobalt. It is considered the most important factor in the maintenance of nerves and also has a number of other important functions within the body, however deficiency and depletion of B12 are prevalent around the world.
VItamin B12 deficiency can affect many bodily systems including neurologic, hematologic, immunologic, vascular, gastrointestinal, musculoskeletal and genitourinary. Symptoms include extreme tiredness / lack of energy, pins and needles, a sore and red tongue, muscle weakness, difficulty walking (eg balance problems), depression, problems with memory, understanding and judgement, paranoia or hallucinations and many more.
In this week’s blog we interview NHS GP Dr Ayan Panja who gives us his insight on the widespread issue of vitamin B12 deficiency, the testing that is currently available in this area and the complications that can potentially arise if deficient in this nutrient.
Dr Panja will be joining Dr Rangan Chatterjee as a panel member at our Cytoplan Practitioner Education Event on July 1st, you can find out more about this event via this link.
Dr Panja, to start things off we wanted to ask what you think the prevalence of B12 deficiency is, and why are there different opinions on prevalence?
The prevalence varies across the globe for obvious dietary reasons. In the UK it is deemed to be between 1-6% and as high as 80% in parts of Asia and Africa. It is more common over the age of 60. The difficulty arises in how we actually define B12 deficiency. Pernicious anaemia is an autoimmune condition and some clinicians only consider that as true deficiency.
On a practical level many GPs and gastroenterologists look at normal ranges from blood tests. It’s more important to think about whether a person’s B12 is functioning properly, even if it is in the ’normal range’. This is where much of the discourse around prevalence arises.
Why are the daily recommended intakes in the UK, US and elsewhere different?
Intake guidelines on B12 (aka cobalamin) differ because there is no one area that is more contentious in medical circles across the globe than that around diet, supplements or vitamins. It is difficult, even in retrospect, to conduct robust studies that could identify how much of a particular vitamin is enough for a population with different ages, genes, ethnicities and lifestyle habits. This makes public health messaging really difficult. The World Health Organisation conducted a technical consultation on folate and B12 deficiencies in 2008 and “recognised the lack of universally accepted cut offs to define deficiency of either vitamin…”. One of the reasons for this is testing methods and their reliability. There are exceptions. Vitamin D testing is a far simpler affair for instance.
In what circumstances are B12 deficiency tests carried out, and what are those tests?
There can be many reasons to check a person’s B12 levels. They include:
- persistent tiredness
- unexplained aches and pain
- neurological symptoms
- food intolerances
- coeliac disease
- memory loss symptoms
- family history of pernicious anaemia
- those on the drug metformin or on potassium supplements
- people who are heavy drinkers of alcohol
- a person with unexplained anaemia.
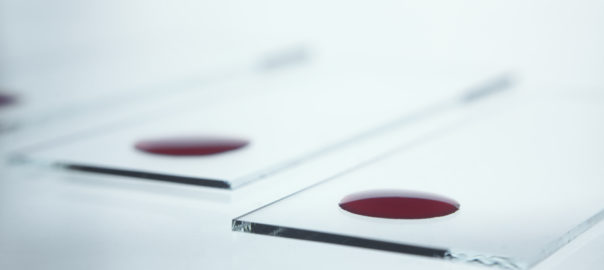
The standard test to measure B12 levels will be a blood test which measures serum B12 levels – that is the amount of B12 that is floating around in the blood, not the amount within the blood cells themselves.
What are the issues and complications around B12 deficiency testing?
It can be hard to get a measure of someone’s level of ‘functioning’ B12. There are other tests which serve as indirect measures of B12 status including methylmalonic acid (MMA) and homocysteine. MMA levels increase when B12 levels drop. Homocysteine is an amino acid which is also raised with low B12 as part of an elegant and critical cellular process which is important for many functions called the methylation cycle. There is much disagreement around the validity of these tests amongst groups of professionals. High homocysteine levels are linked to an increased risk of heart disease, stroke and dementia. My personal view is that sub optimal B12 is under-diagnosed and I have a very low threshold for testing B12 levels.
What is the generally accepted normal B12 range?
In the NHS it is usually 150-900 ng/L but I have seen patients with symptoms of B12 deficiency with levels within these ranges.
Do you think that most GPs understand B12 deficiency properly?
There is still no real consensus on testing. Deficiency can cause so many symptoms from depression, infertility, digestive issues, poor hair and nails, joint pains, cramps – the list goes on. In Cambridgeshire, a NHS neurology team has started giving high doses of intramuscular B12 to those with chronic fatigue as it seems to help. Many of these patients probably have a methylation issue by virtue of their genes. There is a gene mutation affecting MTHFR (an enzyme that converts dietary folate [vitamin B9] into an active form) which can alter how someone processes other B vitamins including B12. Methylation occurs over a billion times a second. I doubt that most GPs would be aware of this gene mutation. I certainly wasn’t until about 3 years ago but it can be a useful test in the right context.
In which circumstances are tablets or injections prescribed?
Tablets are generally not recommended very commonly, as B12 is poorly absorbed from the stomach, especially if the patient has poor absorption. Injections or sublingual sprays or lozenges (under the tongue) work far better.
If someone does not have a B12 deficiency, can they gain an energy boost from a B12 injection?
Yes possibly as it will help the conversion of carbohydrates into glucose that the body can use. It also helps muscle contraction.
Can it help with weight loss, as sometimes claimed?
It is not something that I have come across but possibly because it helps convert carbohydrates into glucose and helps in the breakdown of fats and proteins.
Do you agree with campaigners who are pushing for B12 injections to be made available over-the-counter, and doctors to prescribe more frequent treatment? If so, why?
I think there are too many people out there who have been misdiagnosed and so I totally understand the push for more OTC B12 preparations like injections. There would need to be some governance around training and safety for injectables. There are already sublingual supplements available OTC which is great. I don’t think it’s a bad thing. People can already freely buy drugs like ibuprofen, codeine and paracetamol – which are fatal in overdose. I think if people feel unwell on supplementary B12 then they should seek advice from their GP. I personally would want to know more about their methylation and the form of B12 supplement is key.
What do you think is behind the recent increase in availability of B12 injections in private “clinics”/salons, such as at Harvey Nichols?
For many years, in the USA particularly, intravenous vitamin therapy has been available street corners at “IV Lounges”. They tend to be frequented by anyone from City workers with hangovers to people with chronic fatigue and cancer. It dates back to the era of the Myers cocktail formulated in the 1960s by Dr John Myers from Baltimore who wanted to improve nutrient intake in his patients with poor health. It taps into the modern concept of wellbeing on a number of levels. People are busier than ever with little time to focus on their health. Many want a quick fix of something whilst continuing to carry on with their not so healthy habits.
There’s nothing more ‘medical yet natural’ in people’s minds than an IV vitamin drip. Others who have them may feel let down by conventional medicine or feel that they are not nutrient replete, so find that an IV drip keeps them feeling well whilst dealing with a chronic illness. The absorption of intravenous nutrients is obviously superior compared to oral vitamins. The MHRA will have the final say on how the actual contents of the drips are regulated, as historically many of the products have come in to the UK from outside the EU.
Cytoplan Editor’s notes
With many thanks to Dr Ayan Panja for providing us with his thoughts on the global problem of vitamin B12 deficiency. It is indeed an issue of widespread concern and is one of the most documented and researched nutrient deficiencies in medical science.
If looking to supplement with vitamin B12 then understanding the different forms is particularly important.
Forms of B12
The most commonly found ‘forms’ of B12 used in supplements are cyanocobalamin, methylcobalamin, hydroxycobalamin and adenosylcobalamin. In supplements cyanocobalamin is the most commonly used form despite methylcobalamin and hydroxycobalamin being better absorbed, retained and used by the body.
The inactive cyanocobalamin and hydroxycobalamin forms can be converted to the active cofactor forms – methylcobalamin in the cytoplasm of cells and adenosylcobalamin in the mitochondria.
Cyanocobalamin is an inactive form of B12 and exists only via chemical supplementation. It is not present in nature meaning the body does not metabolically recognise it and absorption is much less efficient.
Hydroxycobalamin is a natural inactive form of vitamin B12 attached to a hydroxyl group. This form can be converted into active methylcobalamin and adenosylcobalamin in the body. For some people this form may be indicated rather than the active methylcobalamin. Hydroxycobalamin has a high affinity to plasma proteins. This property helps to retain the hydroxyl protein complex in the blood stream for a much longer period of time, compared to cyanocobalamin. Hydroxycobalamin may be indicated where high nitric oxide levels are suspected as it is an effective nitric oxide scavenger. Too much nitric oxide can contribute to oxidative stress. Hydroxycobalamin may also be recommended for people who do not tolerate methyl groups.
Methylcobalamin is an active form of B12 where the cyanide group is replaced with a methyl group. It occurs in the cytoplasm of cells and can be synthesised from hydroxycobalamin by the addition of a methyl group. It is needed for vital cellular processes including methylation and DNA synthesis. Thus methylcobalamin is a cofactor in the methionine cycle (methylation cycle). The purpose of this cycle is to regenerate SAM (s-adenosyl methionine) the universal methyl donor.
In the process homocysteine is converted to methionine. Methylcobalamin is the only form able to cross the blood brain barrier without further metabolism, other forms need to be reduced. This form of B12 may be recommended to provide ‘methyl’ groups or for people with specific genetic polymorphisms that can result in less effective recycling of B12. It would also be indicated where an active form is required, for example if it is suspected that there are conversion issues from the inactive hydroxycobalamin form.
Adenosylcobalamin is the mitochondrial form of B12 which acts as a co-factor for a metabolic enzyme involved in energy production. It can be synthesised from hydroxycobalamin or methylcobalamin. People with certain genetic polymorphisms may have a reduced capacity to synthesise adenosylcobalamin. This can result in elevated levels of methylmalonic acid which can be measured in blood or urine and which provides an indirect measure of B12 status.
Genetic mutations
As well as MTHFR mutations, other methylation cycle genes such as MTR and MTRR may affect how B12 is used and recycled; plus TCN mutations can affect B12 transport proteins. Mutations in all these genes can increase the need for B12.
Factors that can contribute to low levels of B12 and deficiency
Vegan or vegetarian diets, damage to parietal cells in the stomach (eg due to gastritis), low stomach acid (eg due to antacid medication), nitrous oxide (used in some surgical operations), genetics, malabsorption (eg Crohns), surgery to stomach/small intestine, some prescription drugs (eg metformin and others).
 Dr Ayan Panja
Dr Ayan Panja
MRCGP, MBBS, DRCOG, DFFP
Dr Ayan Panja has been a doctor for 18 years having qualified from the Imperial College School of Medicine. He works as a GP Partner in St Albans, Hertfordshire and has a keen interest in preventive medicine.
Website: http://www.h21.org.uk/
With many thanks to Dr Panja for taking part in this Q &A session on the topic of vitamin B12 deficiency. If you have any questions regarding the health topics that have been raised, or any other health matters please do contact me (Clare) by phone or email at any time.
Clare@cytoplan.co.uk, 01684 310099
A Cytoplan Practitioner Education Day
Join Dr Rangan Chatterjee and a panel of experienced clinicians to discuss the evolution of lifestyle medicine, and be part of creating the fabric of future primary care in the 21st century. The panel will include this week’s blog interviewee Dr Ayan Panja, Technical Director of Cytoplan Amanda Williams and nutrition practitioner Miguel Toribio-Mateas.
To find out more information, and to book your place, please follow this link.
5 BANT & RCGP CPD hours.
£65 (early bird tickets – £60 until 17th April)
£55 for students
A healthy lunch and refreshments will be provided throughout the day
Last updated on 29th March 2017 by cytoffice



Please tell me can I take B12 with prescribed medications. Amongst others I am on Warfar for life and VK antibiotics.
Hello Roslyn.
Yes you are fine taking the vitamin B12. There are no contraindications between the B12 and the medication that you mentioned.
All the best,
Clare
This article is extremely useful albeit hard to understand all of it. My daughter is vegan and is having bowel problems. She is undergoing investigations atm. Her energy levels are low and she gets low abdo cramps with leg aches and gets wholly headed. When I have spoken to the GP about vit b12 I have been told that she he bloods taken a year ago and her vitb12 was normal so no need to retake it. This concerns me as I am sure something is not quite right. She takes a multi vit most days when I remind her. Any advice or thoughts are most welcome.
Unfortunately as this article mentions, serum B12 levels are not always an accurate indication of B12. Vegans are certainly at risk of low B12 and I would recommend a supplement with good levels (an all round multivitamin / mineral supplement as other nutrients can also be low). You say she is taking a multivitamin most days – perhaps check this and what form the B12 is included in and the amount. Also ensure it includes some iron, vitamin D, iodine which can also be low in vegan diets.
She could also take some additional B12 eg 1000 mcg per day for a few months (if she is taking supplemental B12 however this will affect blood test results so if the GP does agree to a B12 test then it would be better to wait until after the test to supplement, plus she should stop her multivit for a week beforehand). Low B12 can affect energy but low energy can also be due to many other factors (eg low iron and others) so just making this change may not be sufficient to make a different.
You mention gut symptoms and that the doctor is carrying out investigations which is good. Of course gut symptoms may be linked to poor digestion and absorption and could also be contributory factor to the low energy.
There may be suggestions I could make regarding changes to diet etc and other supplement suggestions. If your daughter would like to complete a health questionnaire, we will send some written diet and supplement recommendations. This is a free service. The health questionnaire is available at the following link.
https://www.cytoplan.co.uk/nutrition-advice/educational-literature/health-questionnaire
All my best
Clare
When will all gps have up to date training on b12 deficiency? I have had to resort to self injecting supplies bought from a pharmacy in Germany as my doctor stopped my injections and prescribed tablets instead? She refuses to listen to anything i have to say regarding my own research. I am a member of a support group with over 14000 members and the majority of these people have to deal with the same uneducated unwilling to listen to symptom doctors. Most wont even follow current guidelines. There has to be something that can be done about this people are suffering needlessly is it all down to money? No money to be made from a injectable vitamin. Any advice is appreciated.
Hi Heather,
Thanks for your comment on our blog. Have you come across a book called “Could it be B12? An epidemic of misdiagnoses” by Sally Pacholok and Jeffrey Stuart. As I mentioned in the comment above we do offer a free health questionnaire service. If you complete and return a health questionnaire we will send you some written diet and supplement recommendations.
Best wishes, Clare
Yes i am aware of Sally’s work and i have watched her film! I do not need any advice regarding my own treatment as i unlike my doctor have done my research, i raised some questions in my original post that you have not addressed! It is not me that needs advice its our doctors. Unlike yourself they have no clue on this condition and are harming people with their lack of knowledge. Thanks for responding anyway.
Thank you for your comment. I realise that this is a frustrating issue and unfortunately we are not in a position to be able to comment on the training of GPs. However there is growing interest from GPs in nutrition and functional medicine so hopefully this will begin to change.
Best wishes,
Clare
I have been ‘going downhill’ health-wise for around 12 years. Weak, exhausted, pains in knees (x-ray NAD), falling over, unsteady, bowel problems, now need a carer and my life is severely impacted. Pain in joints, unable to go out alone, gastric problems, I could go on. I had an emergency bowel resection 20 + years ago. On many visits to GP practise since I started to feel so unwell, in the last few years, Iwas told over and over that depression caused the symptoms. Last year my husband/carer spoke in stronger terms than I could to GP. Blood tests reluctantly done showed enlarged red cells and then b12 deficiency. Loading injections and 3-monthly top ups have made no difference to my condition. I really do not want to carry on like this.
Hi Judith,
It may be that you would benefit from a different form of B12 in the injection as you have not responded so far. What form are you taking? If it is hydroxycobalamin, you may be better with methylcobalamin – you would obviously need to return to your GP to request this switch. Methylcobalamin is the active form of B12. I would also suggest that you take a multivitamin and mineral with the full range of other B vitamins. For example, CoQ10 Multi. We do also offer a health questionnaire service that may be of interest to you. If you complete and return a health questionnaire we will send some written diet and supplement recommendations. This is a free service. I hope this is helpful to you.
All the best, Clare
Why are GP’s so far behind the times with all the information that’s out there. ?
What’s more concerning is, the fact that many patients are treated for the symptoms rather than actually finding the root cause, I think even the ”nice guideline” don’t make it clear enough. There is another conference this year, one in London & one in Loughborough. Sally Pacholok & Tracey Witty are two of the many experts to attend.
Thanks for letting us and our readers know about the B12 conference with Sally Pacholok later this year. I have read her book – ‘Could it be B12?’ Best wishes, Clare
My daughter 25yrs has been told she has Fibromyalgia, does not absorbed B12 + Vit D and a Hernia. She is very slight in build and cannot put weight no matter what she eats she is constantly hungry and eats well.
She was dreadfully ill could hardly walk or sit up. She was passing blood and
vomiting blood. Severe joint pain, pins and needles . She had episodes where she lost the feeling in her arms,legs and face. We had to beg for her doctor to give her B12 injection and they gave her Vit D tablets after a fight she has this 3 monthly. She is slightly better but still has the on going issues as above. A neurologist recommended B12 more frequently but doctors have refused this. She has had to give up work due to the fatigue plus all above. The doctor has admitted I had been taken her to them from the age of 12 years with these symptoms (but I had been fobbed off ). We have just booked for a private injection of B12 to see if this gives her an extra boost it’s heart breaking looking at her at times. Also her skin can look very bad red marks and spots but not acne. Can you suggest any other supplements etc. The doctors have implied she anorexia in the past which is miles away from what she is. We are at a loss.
Dear Pauline,
Thank you for posting a question on our blog. As you may have seen previously on the blog comments, we do offer a free health questionnaire service which may be of interest to your daughter. If your daughter completes a health questionnaire we will send her some written diet and supplement recommendations. In the meantime she could consider:
B12 methlcobalamin / adenosylcobalamin – sub-lingual tablet. Some people who have injections, also take a sublingual tablet in between injections. The adenosylcobalamin is the form that is used in the mitochondria (where energy is produced).
Foundation Formula 1 – all round multivitamin and mineral.
P5P Extra – this is a supplement with additional levels of other B vitamins, important for energy.
Acidophilus Plus – Live bacteria, take 1 at bedtime.
Has she had her vitamin D levels tested? The optimal range for vitamin D is 100 – 150 nmol/litre (note that 50 nmol / l is considered adequate). There is a good level of vitamin D in the Foundation Formula 1 but if her levels are very low she may benefit from extra for a period of time (also take advantage of the summer sun – vitamin D can be synthesised between 10.00 am and 2.00 pm on sunny days, so 5-15 minutes without suncream as often as possible, but do not allow skin to redden).
It would be useful to have more information on how her sleep is, gut health etc and her current diet and if you provide this on a questionnaire we can send you further suggestions.
I hope this is helpful.
Best wishes
Clare
Very good sounds like something i need.