Vitamin D plays a critical role in protecting humans from invasive pathogens, reducing the risk of autoimmunity and maintaining optimal health – while low vitamin D levels leave an individual susceptible to infections and developing autoimmunity. This systematic review released last month takes an in depth look into the evidence around vitamin D’s mechanisms and effects on enhancing both innate and acquired immunity – and in this week’s blog we take a closer look at some of the most recent research examining vitamin D’s role in supporting immunity.
But firstly… a little background on vitamin D.
What is vitamin D?
Vitamin D is known as ‘The Sunshine Vitamin’. This is because sunlight is necessary for the synthesis of vitamin D in the skin and those lacking in sunlight are at high risk of deficiency.
Vitamin D is not found in abundance naturally in foods. So simply put, not enough sunshine means not enough vitamin D, and hence issues with widespread deficiency in the UK, particularly in areas such as parts of Scotland that get even less sunshine. The amount of sunlight (UV) in our winter months is insufficient and over the winter we need to draw on our bodily reserves.
There are some foods that can provide us with vitamin D, although it is challenging to obtain good levels from diet alone. According to the Vitamin D Council:
“Fatty fish such as salmon, mackerel, and sardines are rich in Vitamin D. Additionally, fish liver oils, like cod liver oil, provide a high concentration of this nutrient. Many food products are fortified with Vitamin D, including milk, orange juice, and breakfast cereals.1” however, food fortification typically uses vitamin D2 which is not always well absorbed or utilised by the body.
Vitamin D has the following permitted health claims:
Vitamin D contributes to the:
- normal absorption/utilisation of calcium and phosphorus
- normal blood calcium levels
- maintenance of normal bones and teeth
- maintenance of normal muscle function
- normal function of the immune system
- process of cell division
Vitamin D is also needed for normal growth and development of bone in children.
Vitamin D helps to reduce the risk of falling associated with postural instability and muscle weakness. Falling is a risk factor for bone fractures among men and women 60 years of age and older.
Here in the UK, the current government advice is for all adults and children to consider taking a daily 10 micrograms supplement of vitamin D between October and March. Some at-risk groups are advised to consider taking a supplement throughout the year. However, uptake is low with only 1 in 6 adults reporting taking a daily supplement2, and a 2021 survey commissioned by the British Nutrition Foundation found that almost half of Britons are unaware of these recommendations.3
Despite a large percentage of us likely having insufficient levels, those who are at an increased risk of deficiency include:
- infants and children aged 5 and below
- pregnant or breastfeeding women – meeting the mother’s requirements for vitamin D is important as is building adequate foetal stores for early infancy
- those who have darker skin – e.g. people of African, African-Caribbean, or South Asian ethnic origin as the pigment melanin reduces the skin’s ability to make vitamin D in response to sunlight exposure
- overweight or obese people – high prevalence of vitamin D deficiency in obese subjects is well-documented
- those who have reduced exposure to sunshine – such as people who cover their skin or use high factor sunscreen
- the elderly – particularly if they stay indoors during the winter months and especially those who are institutionalised
- those who take certain medications – which can impair vitamin D metabolism
Vitamin D is considered to be deficient if levels are below 29nmol/l. However, optimum levels are suggested to be greater than 125nmol/L.
- Optimal – 125-199 nmol/L
- Sufficient – 75-124 nmol/L
- Low – 30-74 nmol/L
- Deficient – less than 29 nmol/L
If you are unaware of your status or fall into one of the ‘at risk’ categories, then it may be beneficial to get your vitamin D levels tested. Awareness of your vitamin D status means you can focus on attaining optimal results and better health outcomes.
A closer look at some recent vitamin D research
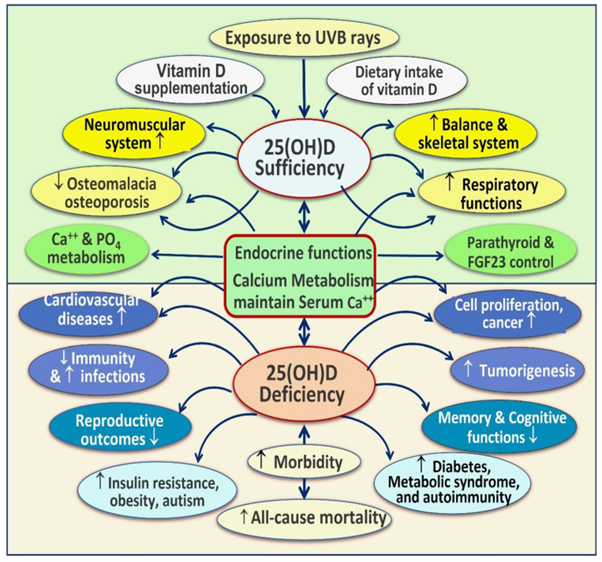
Traditionally seen as a nutrient to support bone health, the far-reaching benefits of vitamin D are becoming ever more apparent. The below image portrays the spectrum of non-skeletal body systems dependent on vitamin D sufficiency for proper functioning, as well as the common disorders that are worsened by chronic vitamin D deficiency, as defined by the evidence outlined in last month’s review.4
The authors comment that vitamin D deficiency is a significant public health problem – a pandemic – that has overtaken iron deficiency as the most common nutritional deficiency globally.
The prevalence of vitamin D deficiency and its associated complications have been escalating over the past three decades, and this study was undertaken, in part, to address this issue.4
Vitamin D and immunity
Vitamin D influences both innate and adaptive immune systems. The action of vitamin D is based on its binding to the Vitamin D Receptor (VDR), a nuclear receptor, which influences gene transcription patterns and which is expressed in the majority of immune cells including monocytes, B cells, T cells, neutrophils and Antigen Presenting Cells (APCs i.e. dendritic cells and macrophages).5 APCs link the innate and adaptive immune systems and present antigens to T cells.6
Vitamin D – innate immunity
Historical evidence that links vitamin D with innate immunity came from the reports in the mid-1800s and early 1900s prior to the antibiotic era that vitamin D3-rich cod liver oil and sunlight exposure were used for treatment of tuberculosis (TB).15
The innate immune system is the body’s first line of defence against pathogens, comprising physical barriers (e.g. epithelium), chemical barriers such as the stomach acid, complement proteins and cellular responses such as those mediated by macrophages, dendritic cells and neutrophils – and vitamin D participates in several of these processes.19
Macrophages and monocytes are cells that reside in every tissue of the body. They engulf dead cells and pathogens and produce immune effector molecules. Upon tissue damage or infection, monocytes are rapidly sent to the tissue, where they differentiate into tissue macrophages.
Through their ability to clear pathogens and instruct other immune cells, these cells have a central role in the immune system.
As part of the innate response, Vitamin D binding to VDR induces the production of antimicrobial peptides (cathelicidins) that are capable of killing pathogens or binding to endotoxin. During viral infections, the lung epithelial cells are capable of converting inactive vitamin D to its active form, leading to increased cathelicidin production.7
Supplementation of vitamin D in those who are deficient has been found to improve cathelicidin production and protection against infection. Vitamin D also upregulates the level of autophagy by monocytes. Thus, research has suggested that the active metabolite of vitamin D “may enhance the antibacterial effects via enhancement of their [macrophages and monocytes] phagocytic and chemotaxis abilities”.6
Multiple studies have shown that vitamin D supports gut integrity and intestinal homeostasis between the host and the gut microbiota.
Vitamin D signaling is shown to increase the viability of intestinal epithelial cells, and alleviate damage from pathogenic bacterial lipopolysaccharide, thus improving gut barrier function, restoring tight junctions, improving permeability and reducing inflammation.16
Moreover, vitamin D has been shown to influence the gut microbiome, which, in turn can influence vitamin D metabolism.26
Vitamin D and adaptive immunity
The adaptive immune system (or acquired immune system) responds slowly to an initial encounter with a pathogen but is able to create immunological memory so that subsequent responses are rapid. It includes T and B lymphocytes (white blood cells).
Various types of T cells include those involved in killing the pathogen (T killer cells), regulating the immune response, i.e. shutting it down once the threat has been neutralised (T regulatory cells), immunological memory cells (T memory cells) and others. B cells produce and secrete antibodies and include a subset involved in immunological memory.
VDR expression increases significantly in activated B and T cells and influences 500 genes which are involved in the proliferation and differentiation of adaptive immunity cells. Importantly, these genes also include ones that inhibit autoimmunity developing.27
Vitamin D and autoimmunity
Vitamin D controls autoimmunity by suppressing adaptive immunity via T- and B-lymphocyte activity, and consequently low levels of vitamin D can lead to a dysfunctional immune system; the prime reason for initiating autoimmune responses.8
On top of this, low serum vitamin D levels have been shown to increase the risk of developing autoimmune conditions, as well as worsening existing conditions.9
The link between vitamin D and autoimmune disease is also supported by both seasonal variation (increase prevalence in children born in spring) and latitude (higher prevalence in northern countries with less UVB radiation).27
There is a growing body of evidence demonstrating that vitamin D deficiency is implicated in the pathogenesis of several different autoimmune conditions including:
- Psoriasis10,11
- Type 1 diabetes12,13
- Multiple sclerosis14
- Inflammatory bowel diseases17,18
- Rheumatoid arthritis19,20
- Lupus24,25
- Hashimoto Thyroiditis28,29
Sources of vitamin D
Vitamin D dietary sources include butter, eggs, oily fish and fortified foods – these sources provide only low levels of vitamin D – most is produced in the skin following sun exposure.
In the UK, vitamin D can be synthesised in the skin between April and September, 10.00 am to 2.00 pm, on sunny days (i.e. without cloud cover). Production also depends on genetics, age, sunscreen, clothing, and skin colour. Although vitamin D cannot be synthesised during the winter at our latitude, it can be stored in the body. Levels are likely to be lowest around March.
With vitamin D supplementation now publicly being recommended, it is important to understand the difference between the most common forms of vitamin D, and which is the most suitable for supplementation.
Choosing the right form of vitamin d supplement
Choosing the correct form of vitamin D to supplement with is just as important as supplementation itself, and although the UK government advising that everyone should take a vitamin D supplement, actual advice in this area has been lacking.
Vitamin D3 vs vitamin D2
Vitamin D3 is the most bioavailable form of this nutrient and far preferable to Vitamin D2 to supplement with.
Vitamin D2 is also known as ergocalciferol and is commonly produced by plants in response to UV radiation. Some fortified foods contain vitamin D2 as an inexpensive addition, however it is not well absorbed or utilised by the body.
Vitamin D3 (also known as cholecalciferol) is the most bioeffective and biologically active form of this nutrient and is found in humans and animals.
So, when choosing a vitamin D supplement, you are looking for vitamin D3 and not vitamin D2. Where you wish to take a multivitamin and mineral that includes Vitamin D3 it is always important to select such a multi-formula with a nutrient content tailored for your age, gender, pre-existing medical conditions, or specifically for children where appropriate.
If you are considering taking a vitamin D3 supplement and a multivitamin, make sure that you assess the total combined dosage of the vitamin that you will be taking.
The importance of cofactor nutrients
The full activity of vitamin D, vitamin D receptors and associated enzyme reactions require the presence of, or the administration of several cofactors.
For example, supplementing with magnesium, another commonly deficient mineral, has shown to improve vitamin D levels, due to the fact that several of the enzymes that synthesise and metabolise vitamin D are magnesium dependent.21
Other necessary cofactors include vitamins A, B2, C and K, antioxidant trace minerals zinc and selenium, resveratrol, essential fatty acids and boron.22 A continuous supply of these nutrients is necessary to attain optimal potentials of vitamin D and better clinical outcomes, so where appropriate, a comprehensive multivitamin and mineral may be advisable.23
Key Takeaways
- Vitamin D is known as ‘The Sunshine Vitamin’ because sunlight is necessary for the synthesis of vitamin D in the skin and those lacking in sunlight are at high risk of deficiency, particularly because rich food sources are scarce
- UK government advice is to consider taking a daily 10 micrograms supplement of vitamin D between October and March. Some at-risk groups are advised to consider taking a supplement throughout the year.
- Traditionally regarded as a nutrient to support bone health, vitamin D also plays an essential role in immunity
- Vitamin D can support both innate and adaptive immunity through a number of mechanisms
- Several autoimmune conditions have been linked to a deficiency in vitamin D
- D3 is the most bioeffective and biologically active form of vitamin D3, so preferred for supplementing and it is important to also consider cofactors such as magnesium
References
- https://www.vitamindcouncil.org/
- New review launched into vitamin D intake to help tackle health disparities – GOV.UK (www.gov.uk) (2022). (Accessed: 25th September 2023).
- 49% adults unaware of vitamin D recommendation – British Nutrition Foundation(2021). (Accessed: 25 September 2023).
- Wimalawansa SJ. Infections and Autoimmunity-The Immune System and Vitamin D: A Systematic Review. Nutrients. 2023 Sep 2;15(17):3842. doi: 10.3390/nu15173842. PMID: 37686873; PMCID: PMC10490553.
- Carlberg C. Vitamin D in the Context of Evolution. Nutrients. 2022 Jul 22;14(15):3018. doi: 10.3390/nu14153018. PMID: 35893872; PMCID: PMC9332464.
- Szymczak I, Pawliczak R. The Active Metabolite of Vitamin D3 as a Potential Immunomodulator. Scand J Immunol. 2016 Feb;83(2):83-91. doi: 10.1111/sji.12403. PMID: 26678915.
- L Bishop E, Ismailova A, Dimeloe S, Hewison M, White JH. Vitamin D and Immune Regulation: Antibacterial, Antiviral, Anti-Inflammatory. JBMR Plus. 2020 Sep 15;5(1):e10405. doi: 10.1002/jbm4.10405. PMID: 32904944; PMCID: PMC7461279.
- Caccamo D, Ricca S, Currò M, Ientile R. Health Risks of Hypovitaminosis D: A Review of New Molecular Insights. Int J Mol Sci. 2018 Mar 17;19(3):892. doi: 10.3390/ijms19030892. PMID: 29562608; PMCID: PMC5877753.
- Sîrbe C, Rednic S, Grama A, Pop TL. An Update on the Effects of Vitamin D on the Immune System and Autoimmune Diseases. Int J Mol Sci. 2022 Aug 29;23(17):9784. doi: 10.3390/ijms23179784. PMID: 36077185; PMCID: PMC9456003.
- Brożyna AA, Slominski RM, Nedoszytko B, Zmijewski MA, Slominski AT. Vitamin D Signaling in Psoriasis: Pathogenesis and Therapy. Int J Mol Sci. 2022 Aug 2;23(15):8575. doi: 10.3390/ijms23158575. PMID: 35955731; PMCID: PMC9369120.
- Barrea L, Savanelli MC, Di Somma C, Napolitano M, Megna M, Colao A, Savastano S. Vitamin D and its role in psoriasis: An overview of the dermatologist and nutritionist. Rev Endocr Metab Disord. 2017 Jun;18(2):195-205. doi: 10.1007/s11154-017-9411-6. PMID: 28176237; PMCID: PMC5486909.
- Yu J, Sharma P, Girgis CM, Gunton JE. Vitamin D and Beta Cells in Type 1 Diabetes: A Systematic Review. Int J Mol Sci. 2022 Nov 20;23(22):14434. doi: 10.3390/ijms232214434. PMID: 36430915; PMCID: PMC9696701.
- He LP, Song YX, Zhu T, Gu W, Liu CW. Progress in the Relationship between Vitamin D Deficiency and the Incidence of Type 1 Diabetes Mellitus in Children. J Diabetes Res. 2022 Sep 2;2022:5953562. doi: 10.1155/2022/5953562. PMID: 36090587; PMCID: PMC9463035.
- Smolders J, Torkildsen Ø, Camu W, Holmøy T. An Update on Vitamin D and Disease Activity in Multiple Sclerosis. CNS Drugs. 2019 Dec;33(12):1187-1199. doi: 10.1007/s40263-019-00674-8. PMID: 31686407; PMCID: PMC6890630.
- Charoenngam N, Holick MF. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients. 2020 Jul 15;12(7):2097. doi: 10.3390/nu12072097. PMID: 32679784; PMCID: PMC7400911.
- Lee C, Lau E, Chusilp S, Filler R, Li B, Zhu H, Yamoto M, Pierro A. Protective effects of vitamin D against injury in intestinal epithelium. Pediatr Surg Int. 2019 Dec;35(12):1395-1401. doi: 10.1007/s00383-019-04586-y. Epub 2019 Oct 14. PMID: 31612340.
- Battistini C, Ballan R, Herkenhoff ME, Saad SMI, Sun J. Vitamin D Modulates Intestinal Microbiota in Inflammatory Bowel Diseases. Int J Mol Sci. 2020 Dec 31;22(1):362. doi: 10.3390/ijms22010362. PMID: 33396382; PMCID: PMC7795229.
- Vernia F, Valvano M, Longo S, Cesaro N, Viscido A, Latella G. Vitamin D in Inflammatory Bowel Diseases. Mechanisms of Action and Therapeutic Implications. Nutrients. 2022 Jan 9;14(2):269. doi: 10.3390/nu14020269. PMID: 35057450; PMCID: PMC8779654.
- Harrison SR, Li D, Jeffery LE, Raza K, Hewison M. Vitamin D, Autoimmune Disease and Rheumatoid Arthritis. Calcif Tissue Int. 2020 Jan;106(1):58-75. doi: 10.1007/s00223-019-00577-2. Epub 2019 Jul 8. PMID: 31286174; PMCID: PMC6960236.
- Lee YH, Bae SC. Vitamin D level in rheumatoid arthritis and its correlation with the disease activity: a meta-analysis. Clin Exp Rheumatol. 2016 Sep-Oct;34(5):827-833. Epub 2016 Apr 6. PMID: 27049238.
- Dai Q, Zhu X, Manson JE, Song Y, Li X, Franke AA, Costello RB, Rosanoff A, Nian H, Fan L, Murff H, Ness RM, Seidner DL, Yu C, Shrubsole MJ. Magnesium status and supplementation influence vitamin D status and metabolism: results from a randomized trial. Am J Clin Nutr. 2018 Dec 1;108(6):1249-1258. doi: 10.1093/ajcn/nqy274. PMID: 30541089; PMCID: PMC6693398.
- Wimalawansa, Sunil. (2020). Reducing Risks from COVID-19: Cost-Effective Ways of Strengthening Individual’s and the Population Immunity with Vitamin D. Journal of Endocrinological Science. 2. 10.29245/2767-5157/2020/2.1112.
- Wimalawansa S.J. Fighting against COVID-19: Boosting the immunity with micronutrients, stress reduction, physical activity, and vitamin D. Food Sci. J. 2020;3:126.
- Charoenngam N. Vitamin D and Rheumatic Diseases: A Review of Clinical Evidence. Int J Mol Sci. 2021 Oct 1;22(19):10659. doi: 10.3390/ijms221910659. PMID: 34639000; PMCID: PMC8508879.
- Dall’Ara F, Cutolo M, Andreoli L, Tincani A, Paolino S. Vitamin D and systemic lupus erythematous: a review of immunological and clinical aspects. Clin Exp Rheumatol. 2018 Jan-Feb;36(1):153-162. Epub 2017 Nov 14. PMID: 29148401.
- Yamamoto EA, Jørgensen TN. Relationships Between Vitamin D, Gut Microbiome, and Systemic Autoimmunity. Front Immunol. 2020 Jan 21;10:3141. doi: 10.3389/fimmu.2019.03141. PMID: 32038645; PMCID: PMC6985452.
- Martens PJ, Gysemans C, Verstuyf A, Mathieu AC. Vitamin D’s Effect on Immune Function. Nutrients. 2020 Apr 28;12(5):1248. doi: 10.3390/nu12051248. PMID: 32353972; PMCID: PMC7281985.
- Zhao R, Zhang W, Ma C, Zhao Y, Xiong R, Wang H, Chen W, Zheng SG. Immunomodulatory Function of Vitamin D and Its Role in Autoimmune Thyroid Disease. Front Immunol. 2021 Feb 19;12:574967. doi: 10.3389/fimmu.2021.574967. PMID: 33679732; PMCID: PMC7933459.
- Kim D. The Role of Vitamin D in Thyroid Diseases. Int J Mol Sci. 2017 Sep 12;18(9):1949. doi: 10.3390/ijms18091949. PMID: 28895880; PMCID: PMC5618598.
If you have questions regarding the topics that have been raised, or any other health matters, please do contact our team of Nutritional Therapists.
nutrition@cytoplan.co.uk
01684 310099
Last updated on 3rd January 2024 by cytoffice



Love the article, thank you! Can you share the source for the optimal levels quoted? Thanks
Hi there – these figures have been obtained from the plethora of literature available on the benefits of Vitamin D. For example, in the systematic review mentioned, they comment that “Based on the data, it is also reasonable to contemplate that the minimum serum 25(OH)D concentration needed for a healthy life for all ages of humans is 50 ng/mL” – this equates to the 125nmol/L we list as being the beginning of optimal levels.
A great informative article … do this for all your products …it educates us quickly and effectively when we’re trying to figure out a correct answer to our failing health ….and the essential references are a bit more reassuring .increasing the likelihood that it may well help provide the correct answer to an ailment. You cant rely on the Gods of Medicine.
Thank you for your kind feedback.